L5-Patho Peptic Ulcer Disease
Anatomy & Physiology
Normal Stomach
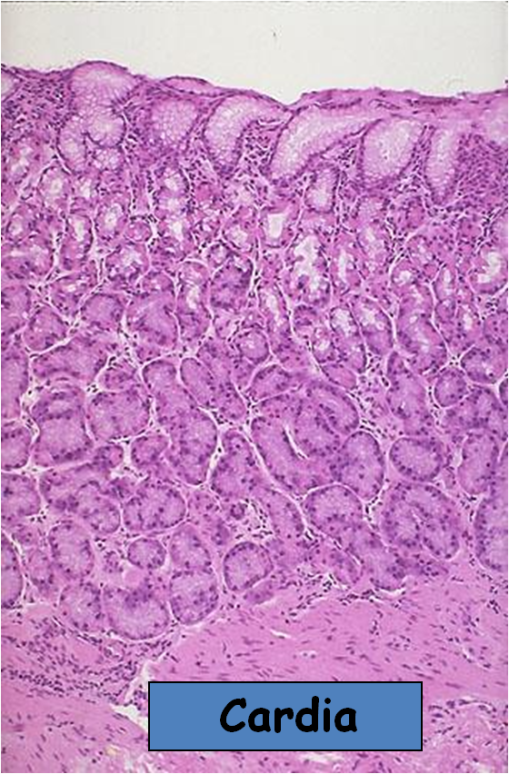
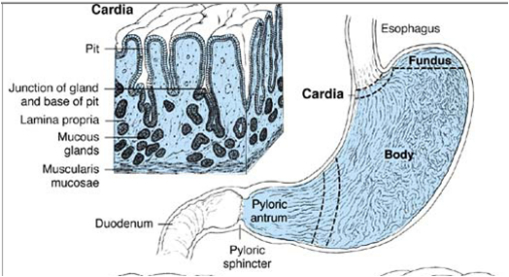
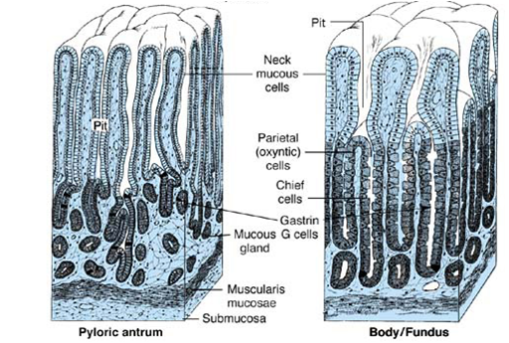
1) Cardia – mucus cells only
2) Body: Parietal (HCL+ intrinsic factor) and Chief cells (pepsin)
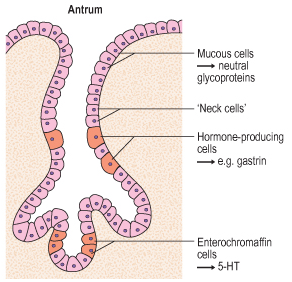
3) Antrum: Mucin secretion and G-cells that secrete gastrin
Stomach
Pathology of Peptic Ulcer Disease
Acute gastritis “gastropathy”
– Injury to the gastric mucosa (Hyperemia and erosions) with no significant participation of inflammatory cells
Causes include:
– Non-steroidal anti-inflammatory drugs (NSAIDs)
– Alcohol
– Hypovolemia
– Shock
– Stress (burns, surgery, strokes, post infarction)
– Uremia
– Cancer chemotherapy
– Enterogastric reflux
– Corrosives (may cause perforation)
– Acute gastritis is a major cause for hematemesis especially in alcoholics.
– 25% of persons who take daily aspirin for Rh arthritis develop acute gastritis at one point.
– Erosions affect the superficial mucosa and can heal rapidly as opposed to ulceration.
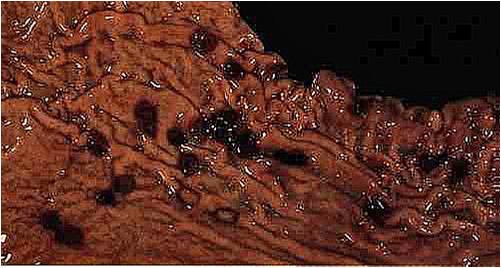
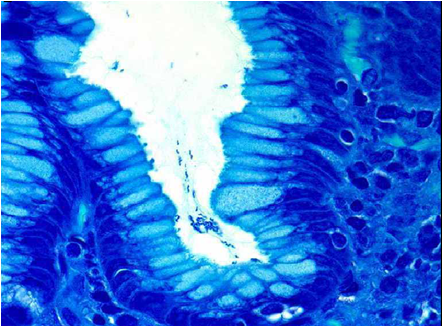
Acute errosive gastritis
The superficial part of the epithelium is only affected
Chronic Gastritis
– Chronic gastritis is defined histologically as an increase in the number of lymphocytes and plasma cells in the gastric mucosa.
– The mildest degree of chronic gastritis is chronic superficial gastritis, which involves the subepithelial region around the gastric pits.
-More severe cases involve the glands in the deeper mucosa; this is commonly associated with gland atrophy (chronic atrophic gastritis) and intestinal metaplasia.
Causes:
1- Autoimmune:
-auto-antibodies to parietal cells (decreased acid and intrinsic factor)
-Type A chronic gastritis
2- Helicobacter pylori:
-G-ve bacilli; Noble prize in Medicine 2005, for Barry Marshal & Robin Warren
-Type B chronic gastritis
-Helicobacter pylori is present in 70-90% of patients with gastric and duodenal ulcers, respectively
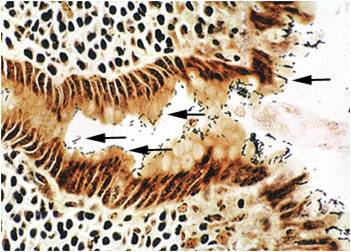
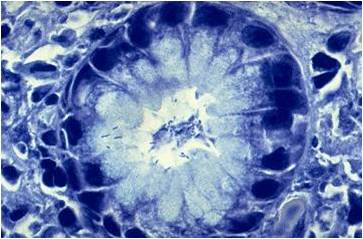
Chronic Superfecial gastritis
Chronic atrophic gastritis
Types of chronic gastritis
– Most cases of chronic gastritis are of one of two types
1- type A, which is an autoimmune gastritis that primarily involves the body and is associated with pernicious anemia;
2- type B, which primarily involves the antrum and is associated with Helicobacter pylori infection.
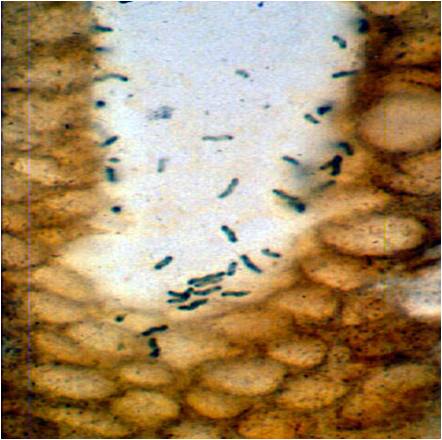
Helicobacter pylori
Mechanisms of H. pylori-induced pathology
– Although the organism is not invasive, it induces intense inflammatory and immune response: cytokines and B-cell activation
– Enhances gastric acid secretion
– Bacterial products such as urease, lipases and proteases induce epithelial injury
Helicobacter pylori associated disorders
1-Chronic gastritis
2- Peptic (gastric and duodenal) ulcers
3- Gastric adenocarcinoma, intestinal type
4- Gastric lymphoma
H. pylori
Gastric ulcer
Relation between helicobacter and duodenal ulcers
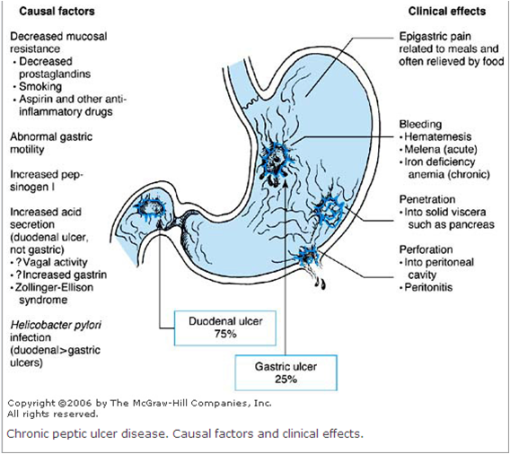
Chronic Peptic ulcer
– Peptic ulcers are ulcers occurring in any part of the gastrointestinal tract exposed to the action of acidic gastric juice. These include
1- First part of duodenum
2- Stomach
3- Lower esophagus
4- Meckel’s diverticulum
5- Stomal (marginal) ulcer (gastro-jujenostomy)
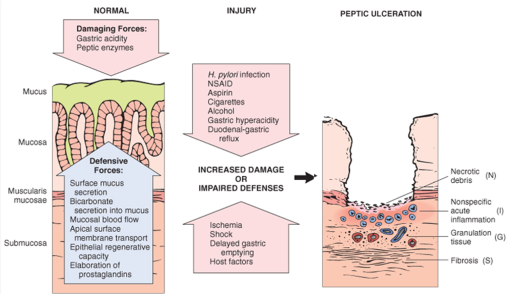
Pathogenesis
-The gastric mucosa is protected by a variety of mechanisms from the erosive effect of gastric acid, these include
1-The anatomic integrity of the mucosa:
-The mucosal cells have a specialized apical surface membrane that resists the diffusion of acid into the cell.
2-Gastric mucus:
-Mucin and HCO3 secreted by surface epithelial cells create a mucous layer that has a pH gradient which is very acid in the lumen to nearly neutral near the cell surface.
3- Prostaglandins (E series):
-which are synthesized and secreted by gastric mucosal cells, have a cytoprotective effect on the gastroduodenal mucosa. They act to increase bicarbonate secretion, gastric mucus production, mucosal blood flow, and the rate of mucosal cell regeneration.
4- Mucosal blood flow:
-Ischemia of the mucosa decreases mucosal resistance.
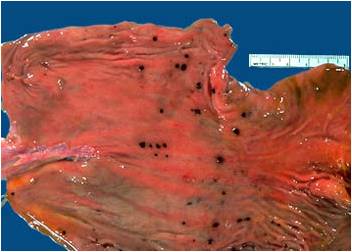
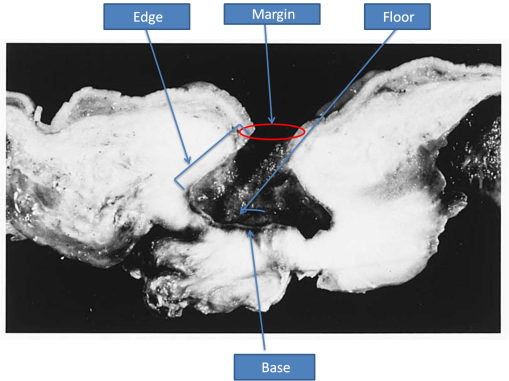
Peptic ulcer- Morphology (gross)
Chronic peptic ulcers are
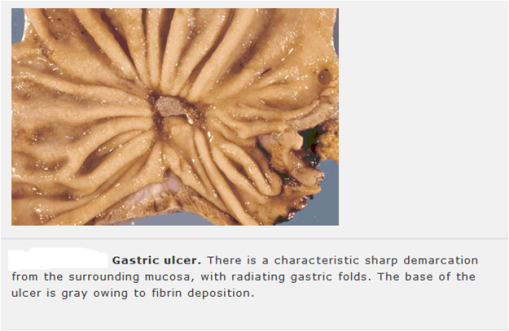
1-Usually solitary, round-to-oval in shape
2- Often large (larger than 1 cm, rarely larger than 5 cm) and usually found on the lesser curvature or pyloric antrum
3- Margins are either flush with the mucosal surface or slightly raised because of edema. The edge is punched out, the floor of the ulcer is smooth, and its base is thick and firm because of fibrosis.
4- The mucosa around the ulcer is either normal or—in the stomach—shows changes of chronic gastritis.
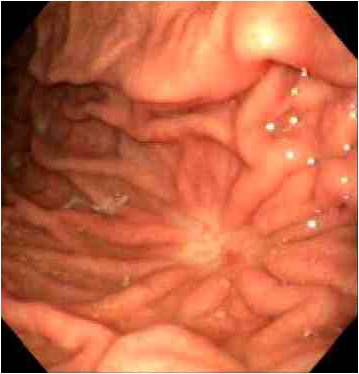
5- The mucosal folds around the ulcer appear to radiate outward from it, which is an effect of fibrous contraction of the base of the ulcer
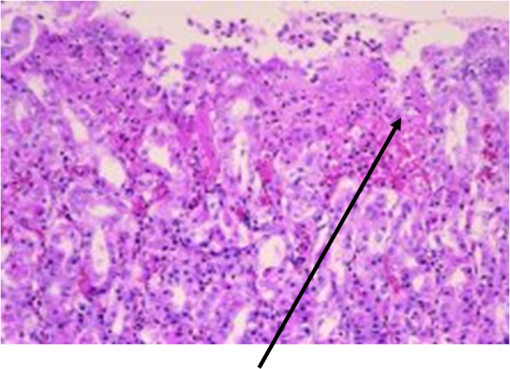
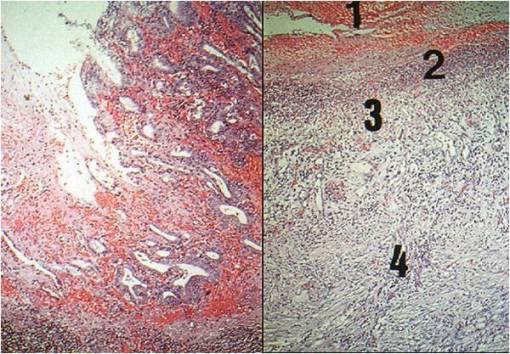
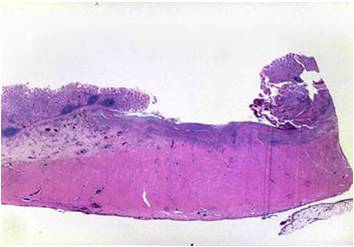
Peptic ulcer- Morphology (micro)
Microscopically, the base of a chronic peptic ulcer is composed of :-
1- A surface of necrotic layer
2- Acutely inflamed layer
3- A zone of granulation tissue.
4- Extensive fibrosis of the base, with extension of fibrosis into the muscle wall.
5- The epithelium at the edge of the ulcer shows regenerative hyperplasia, which frequently demonstrates marked cytologic atypia, mimicking neoplastic change.
Peptic ulcer-Complications
Clinical features:
Epigastric pain (worse at night and relieved by food), bleeding (30%) and perforation (5%; accounts for 2/3 of deaths).
Complications:
1- Hemorrhage
2- Perforation, penetration.
3- Fibrosis – stenosis, hour-glass stomach
4- Duodenal diverticulum
5- Malignancy, rare, gastric not duodenal















No trackbacks yet.