Your Medical Frontline
Archive for the ‘ Case 3 (COPD) ’ Category
L4- Antibiotic Therapy of Lober Pneumonia
What Are the Frequent Causative Organisms Of Lober Pneumonia ?
TYPES OF PNEUMONIA DRUG
# Antimicrobial
# Antibiotic
# Chemotherapeutic agent
1) ANTIMICROBIALS
Classification
I. According to mechanism

II. According to antimicrobial activity
•Narrow spectrum
•Broad spectrum
•Wide spectrum
III.According to cidal and static activities
I-Bacteriostatics
1-Macrolides
2-Chloramphenicol
3-Tetracyclins
4-Sulfonamides
II-Bactericidals:
1-Beta Lactams
- Cephalosporins
- Penicillins
2-Aminoglycosides
3-Quinolones
4-Rifampicin
•Indications of bactericidal agents:
Severe cases
Debilitated patients
Agranulocytosis
Aplastic anaemia
+ Immunosuppression
Factors affecting the antibacterial activity:
I. Concentration at site of infection
II. Bacterial resistance
III. Host defense mechanisms
IV. Local factors
How to minimize the emergence of resistance ?
1.High level maintainance
2.A.B. Combinations
3.Use restriction of valuable drug
General adverse reactions:
1.Hypersensitivity reactions
2.Toxic or irritative effects
3.Super infection (opportunistic infection)
4.Organ toxicities
General principals of antimicrobial therapy:
1.When necessary
2. Susceptibility test
3.Consideration of Ph.K. & hepatic and renal states
4.Loading dose & cidality in serious infection
5.Continuation 3 days after apparent cure to avoid relapse
6.Adequate dose & duration & combined therapy to avoide emergence of resistance
7.Test of cure
8.Avoid abuse
2) Antibiotic
How To Make a Proper Choice Of Antibiotic For Lober Pneumonia ?
1. For Emperical Treatment
2. For Definitive Treatment
What Are The Proper Antibiotics For Lober Pneumonia ?
1.Beta-Lactam Antibiotics
i-Penicillins
Classification
I-Natural:
Pen. G:
– Benzyl Pen.G
– Procaine Pen.G
II-Semisynthetic
1.Antistaph
Cloxacillin
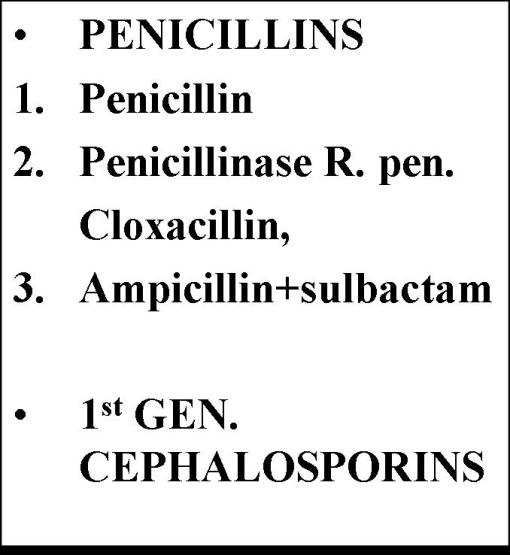

2.Broad S.
Ampicillin
Amoxicillin
3.Extended S.(Anti-pseudomonas)
Carbenicillin
4.Rev.S
Pevmecillinam
What are the contraindications of Penicillins ?
II- Cephalosporins
Similarities to penicillin:
1.A peptide nucleus (7-amino-cephalosporanoic acid)
2.Inhibition of the transpeptidase of the cell wall.
3.Destroyed by a specific bacterial B-lactamase (cephalosporinase)

2.Macrolides (Erythromycin,Azithromycin, Clarithromycin)
•Bind to 50 S ribosomal subunit ( site of chloramphenicol & clindamycin)
•Wide spectrum
•Baceriostatic or bactericidal ( depending on the conc. )
•They accumulate in the macrophages but have no effect on the immune mechanism.
Macrolides are wide spectrum antibiotics ; Mention why ?
Wide spectrum :
= gm.+ve : cocci ( strept., staph., pneumococci)& bacilli ( diphtheria)
= gm- ve : cocci ( Neisseria ) & bacilli (including Helicobacter, H. influenza , Legionella )
=Chlamydia, Mycoplasma, Spirchates and Toxoplasmosis
Adverse effects:
1.G.I upsets, colic
2.Reversible cholestatic hepatitis
3.Allergy
3.Quinolones
How Quinolones act ? How can bacteria resist ? Does it work on human cell ?
Inhibit DNA gyrase
Quinolones spectrum:
–Most gm –ve:
- E-coli
- Proteus
- H.influenza
- Shigella
- Chlamydia
- Klebsiella
- Pseudomonas
- Salmonella
- Legionella
– Gm +ve :
- Strept
- Pneum.
- staph.
Quinolones Contraindications:
1.Prgnancy & nursing mothers
2.Children under 18 years
3.Epilepsy
What are the causes of failure of antimicrobial therapy ?
1.Wrong route
2.Impaired defense
3.Poor penetration
4.Wrong culture
5.Pus
6.Foreign body
7.Delay
8.Sub optimal dose
9.Sub optimal duration
L3- Chronic Obstructive Pulmonary Diseases (COPD)
Chronic Obstructive Pulmonary Diseases (COPD)
A group of pulmonary diseases characterized by increased resistance to air flow due to partial or complete obstruction at any level.

(l) Chronic Bronchitis
It is persistent productive cough (cough of sputum) for at least 3 consecutive months in at least 2 consecutive years.
Causes:
Due to chronic irritation of the bronchial mucosa by:
1- Cigarette smoking.
2- Atmospheric pollution
3- Chronic inflammation of upper respiratory tract, tonsils or mouth.
Pathology:
Occur in middle-aged men.
N/E:
Bronchial mucosa appears thick, opaque and covered by excess mucous.
M/E:
1) Epithelium:
a- Bronchi:
– Goblet cell hyperplasia and decreased number of ciliated cells.
– Squamous metaplasia and dysplasia.
b- Brochioles:
Goblet cells metaplasia
2) Subepithelial Tissue:
chronic inflammatory cell infiltrations.
Bronchial mucous glands are hyperplastic, hyperactive with progressive fibrosis.


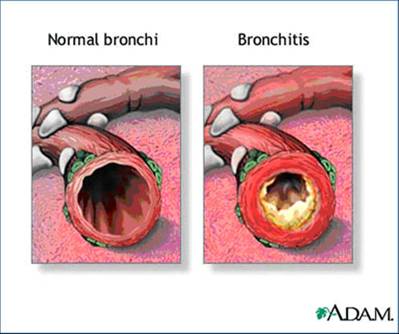
Complications:
1- Centrilobular emphysema.
2- Bronchopneumonia.
3- Bronchogenic carcinoma.
4- Chronic hypoxaemia resulting in persistent pulmonary vasoconstriction, pulmonary hypertension and cor pulmonale.
5- Cardiac failure.
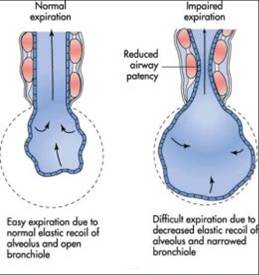
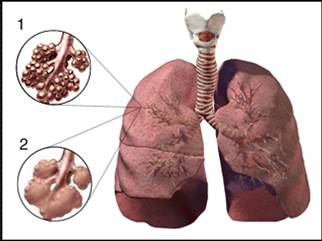
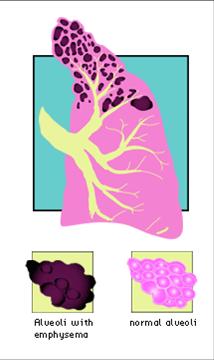
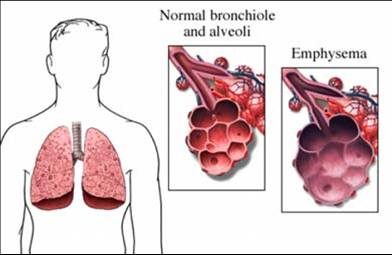
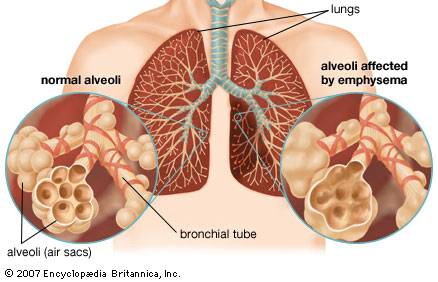
(2) Emphysema
Permanent dilatation of air spaces distal to the terminal bronchioles accompanied by damage of their walls.
i.e. respiratory bronchioles, alveolar ducts and alveoli (respiratory acinus).
Incidence:
The commonest chronic lung disease. It occurs more in males from 40-60 years of age.

A- Centriacinar (Centrilobular):
It involves respiratory bronchiole (central part of acinus).
Pathogenesis:
It is related to cigarette smoking and it is explained by the following theories:
1) Elastase – antielastase imbalance theory
Smoking weakens the walls of air spaces by increasing elastase and inhibiting antielastase
2) Direct Damage Theory:
The walls of air spaces are injured directly by toxic substances of cigarette smoking.
3) Chronic Bronchitis theory:
a- Smoking recruits neutrophils and macrophages and stimulates the release of elastase from them.
b- It increases mucus secretion leading to mucus plugs which partially obstruct the bronchi and Terminal bronchioles. During expiration the air is entrapped and increases gradually the intraluminal pressure.
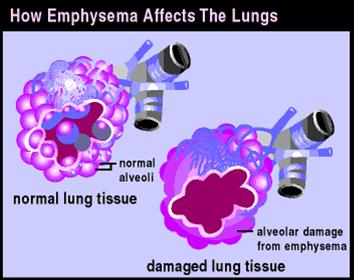

B- Panacinar( Panlobular):
It involves the whole acinus and occurs more in old females.
Pathogenesis:
Related to inherited deficiency of antielastase (a1 antitrypsin) in the patient’s blood. Therefore the action of elastase secreted from neutrophils and macrophages becomes unopposed.
N/E
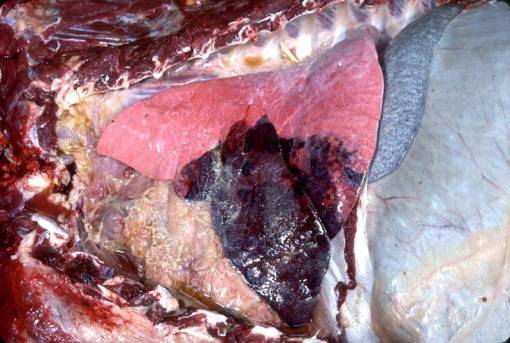
A- Centriacinar emphysema:
Upper zones of the lung lobes are first affected.
The lungs are moderately enlarged.
The affection is mainly centrally located in the acinus (RB)
C/S:- Enlarged air spaces, which are seen in clusters at the center of the lung acinus.
B- Panacinar emphysema:
1) Barrel shaped chest:
The chest wall takes a fixed exaggerated inspiration position:
a- The anteroposterior diameter increases to equal the transverse. The sternum is pushed forward and moderate kyphosis occurs.
b- The ribs, costal cartilages and the intercostal spaces are horizontal.
c- The subcostal angle is wide.
2) Lungs:
Lower zones of lung lobes are first affected.
The lungs are voluminous and very light
They are pale and dry .
The surface is smooth and presents the indentations of ribs.
Lungs have a feathery feeling and pit on pressure (due to loss of elastic tissue).
Large bullae project on the surface in the poorly supported parts (along apices, anterior margin and free edge of base).
A bulla is an emphysematous space of more than 1 cm in diameter, it is semitranslucent with paper – thinned walls.
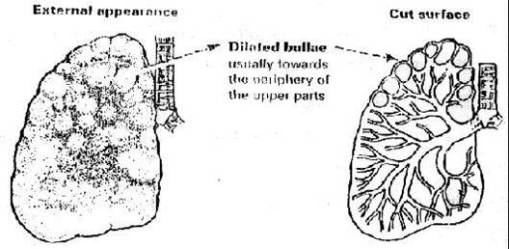
Centrilobular emphysema




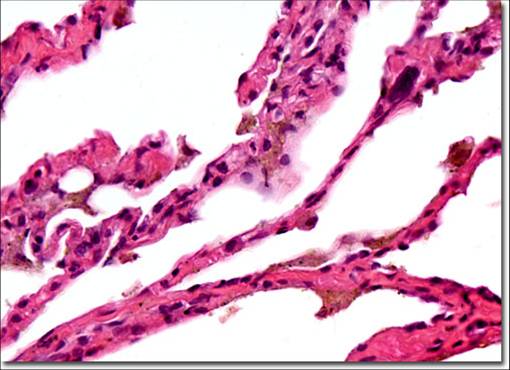
M/E:
A) Centrilobular emphysema·
Dilated respiratory bronchioles (R.B.) with normal A.D. and alveoli.
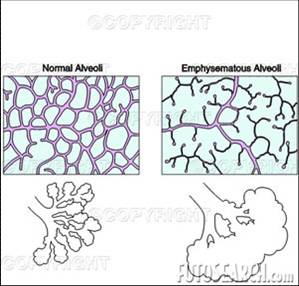
B) Panacinar emphysema.
1) Alveoli are:
Few in number, increased in size, distorted in shape.
2) Interalveolar septa:
Thin and in advanced stages, alveolar septa rupture.
The interalveolar capillaries are compressed by dilated air spaces.


Complications:
1) Respiratory system:
Ch. bronchitis.
Interstitial emphysema.
Spontaneous pneumothorax
Respiratory failure.
2) C. V. S:
pulmonary hypertension and right sided heart failure.
I- Obstructive Hyperinflation (emphysema)
II- Compensatory Hyperinflation (Emphysema)
III- Senile (Atrophic) hyperintlation (emphysema)
IV- Interstitial Emphysema:
(3) Pneumonitis
Inflammation of lung tissue.
Classification
1) Bacteria1:
– Lobar pneumonia.
– Bronchopneumonia
2) Primary Atypical Peneumonitis
3) Loeffler’s Pnueumonia
4) Granuloma
5) Lipid Pneumonia
6) Irradiation Pneumonia
A- Lobar Pneumonia
Acute bacterial infection involving at least an entire lobe of lung (due to streptococcus pneumonia in 95 % of cases)
Incidence:
It predominates in middle-aged males.
Method of infection:
By inhalation. (droplet infection)
Pathogenesis:
1- Exogenous or endogenous pneumococci are inhaled to reach alveoli.
2- They settle into lower lung lobes and one or both sides are involved.
3- Micro-organisms in alveoli produce an inflammatory reaction with fluid exudate.
4- it pass from one alveolus to another through inter- alveolar pores to involve the whole lobe and the pleura.
5- The fluid together with the cellular exudate expel air away from the alveoli producing a firm airless lobe leading to consolidation (hepatisation) of the affected lobe.
Pathology:
Sero-fibrinous inflammation of lung that passes in the following stages.
l) Stage of congestion (1-2 days):
N/E:
1- The involved lobe is:
– Enlarged, dark red and heavy.
– Wet sponge in consistancy.
2- Cut surface: exudes a frothy serous fluids
M/E:
1- Inter-alveolar capillaries are congested
2- Alveoli contain oedema, some air, bacteria and scattered neutrophils.
2) Stage of red hepatization (2 – 4 days):
N /E:
1-The affected lobe:
– Enlarged, red and heavy.
– firm and airless (like the liver)
2- Cut surface: dry and granular.
3- Serofibrinous pleurisy.
4- Hilar L. N. are enlarged (inflamed).
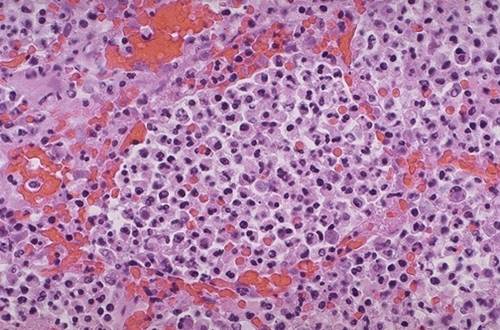
M/E:
1- Inter-alveolar cappillaries still congested.
2- The alveoli are filled with exudate formed of fibrin network entangling in its meshes excess neutrophils, R.B.Cs., few macrophages with bacteria.
3) Stage of grey Hepatization (4-8 days) :
N/E:
1. Affected lobe:
- Enlarged and grey in colour
- Firm and airless (like the liver)
2. Cut surface: dry and granular.
3. Fibrinous pleurisy.
4. Hilar lymph nodes are enlarged.
M/E:
1-Inter-alveolar capillaries: less congested.
2- Alveoli contain:
– Fibrin threads in the center (fibrin retracts give a clear zone adjacent to alv. walls).
-Most inflammatory cells are dead and progressively disintegrat.
-Most micro-organisms are dead and disappear
-Macrophages increase in number.
3- Fibrinous pleurisy
4) Stage of Resolution (8 – 21 days):
Occur in uncomplicated cases:
– Exudate within the alveoli is gradually liquified by fibrinolytic enzymes of inflammatory cells. It is reabsorbed through lymphatics or blood vessels or removed by macrophages and rarely coughed up.
N/E:
1- The affected lobe:
– The size decrease gradually until it becomes normal with restoration of the normal color.
– The consistency becomes as wet sponge and is finally airful.
2- Cut surface: Wet, smooth and exudes a frothy creamy fluid.
3- Pleurisy resolves.
4- Hilar lymphadenitis disappears.






M/E:
Mild or no congestion of inter-alveolar capillaries.
The alveoli contain liquified inflammatory exudate and increased number of macrophages.
Lastly the affected lobe appears normal.

Complications :
1) Pulmonary (in the lung):
Delayed resolution.
Fibrosis, Lung abscess and gangrene.
2) Extrapulmonary (outside lungs):
Spread of infection to pleura (Direct, lymphatic and Blood spread)
Toxaemia.
Clinical course:
7-9 days and terminates by crisis (sudden improvement).
B- Bacterial Bronchopneumonia
Acute bacterial infection of the bronchioles and the surrounding alveoli.
Aetiology:
1) Staphylococcus aureus.
2) Streptococcus pyogens.
3) Pneumococous.
4) haemophilus influenza
Mode of infection: by inhalation.
Types:
1) Primary bronchopneumonia:
Due to 1ry (exogenous) invaders.
Extremes of age.
2) Secondary bronchopneumonia:
Due to 2ry (endogenous) invaders which complicate other diseases.
Pathology :
Acute suppurative inflammation of bronchioles and surrounding alveoli.
N/E:
Multiple patches of consolidation, distributed through several lung lobes or one lobe.
Commonly present in lower lobes (basal) of both lungs (bilateral)
They are better felt than seen.
They are centered around the bronchioles.
Cut surface of a patch is slightly elevated, dry, granular, gery red to yellow and exudes pus on pressure.
Areas between the patches are either normal, collapsed or emphysematous.
Pleurisy is not a marked feature, as the patches do not usually contact the pleura.




M/E:
Patchy affection of bronchioles and surrounding alveoli of acute suppurative bronchiolitis at different stages of development. .
The surrounding alveoli are filled with pus rich in inflammatory cells and pus cells.
Interalveolar septa are acutely inflamed.


Complications:
1. In lung:
Lung abscess and gangrene.
Lung fibrosis, leading to pulmonary hypertension and right-sided head failure.
Bonchiectasis.
2. In pleura:
Empyema
3. Outside the lungs:
a- Spread of infection:
– Direct.
– Lymphatic spread.
– Blood spread.
b- Due to toxaemia:
Clinical course: 2-3 weeks and terminates by lysis.
My Blog My Rule
Blog Stats
- 322,266 hits
| S | M | T | W | T | F | S |
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |||
| 5 | 6 | 7 | 8 | 9 | 10 | 11 |
| 12 | 13 | 14 | 15 | 16 | 17 | 18 |
| 19 | 20 | 21 | 22 | 23 | 24 | 25 |
| 26 | 27 | 28 | 29 | 30 | 31 | |
Mansoura Manchester Medical Programme
- Islam
- Fiqh
- Global Issues
- Hadith
- Kitab
- Palestinaku
- Pra-Muraqazah
- Sautun Nahdhah (Suara Kebangkitan)
- SN001 – 28 Rejab Hari Kejatuhan Khilafah
- SN002 – Susah Sangatkah Untuk Bersatu
- SN003 – Buang Bayi – Natijah Dari Dibuangnya Hukum ALLAH!
- SN004 – YA ALLAH! Demi Ramadhan Yang Mulia Ini, ENGKAU Hancurkanlah Pemimpin Yang Jahat Dan Berilah Kemenangan Kepada Pejuang Agamamu
- SN005 – Tanpa Khilafah,Islam Terus Dihina
- SN006 – Nyawa Hilang Nilai Hasil Penolakan Sistem Islam
- SN007 – Halatuju Politik Baru, Menghala Ke Mana?
- SN008 – Islamic Fashion Festival (IFF) Menghina Islam!
- SN009- Mahukah Anda Berzina Dengan Ibu Sendiri?
- SN010 – Amerika Ditatang,Islam Ditentang!
- SN011 – PILIHANRAYA : Sampai Bila Akan Menjadi Topeng Demokrasi
- SN012 – Hijrah Rasullullah Adalah Keluar Dari Darul Kufur Menuju Darul Islam
- SN013 – WIKILEAKS: Antara Bukti Kejahatan Pemimpin Dan Tajassus
- SN014 – Cabaran Dan Tentangan Sejurus Berdirinya Khilafah
- SN015 – Muhasabah Terhadap Harakah Islam Yang Mengakui Sistem Taghut
- SN016 – Tunisia Perlukan Khilafah, Bukan Sekadar Pertukaran Pemimpin
- SN017 – Mesir Bangkitlah Menuju Perubahan Hakiki Dengan Khilafah
- SN018 – Seruan Hizbut Tahrir Kepada Majlis Tertinggi Angkatan
- SN019 – Mempersiapkan Suasana Thalabun Nusrah Untuk Meraih Kekuasaan
- SN020 – Arab Saudi Dan Pengkhianatan Keluarga Saud
- SN021 – Kekejaman Diktator Libya & Keengganan Para Penguasa Kaum Muslimin Menolong Libya
- Sirah
- Tazkirah
- Tokoh2 Islam
- MMMP
- Sem 1 (Foundation)
- Case 1 (Chem of Life)
- Case 2 (Cell Structure)
- Case 3 (Active & Passive Movement)
- Case 4 (Transcription @ Translation)
- Case 5 (Vitamins,Fat & Water)
- Case 6 (Digestion & Absorption)
- Case 7 (Changes in Electrical Activity Caused by Damage)
- Case 8 (Lung Function,Environment & Epidemiology)
- Case 9 (Inherited Disease)
- Case Ten (Chemistry of Sugar)
- Pract/Osce
- Unseen Case (How's The Body is Regulated)
- Sem 2 (Life Cycle)
- Case 01 (Normal Pregnancy)
- Case 02 (Congenital Heart Disease)
- Case 03 (Thalassemia)
- Case 04 (Hypogonadism)
- Case 05 (Immunodeficiency-HIV/AIDS)
- Case 06 (Autoimmune-SLE)
- Case 07 (Autoimmune-Rheumatoid Arthritis)
- Case 08 (Breast Cancer)
- Case 09 (Osteoporosis)
- Case 10 (Menopause)
- Unseen Case (Ambiguous Genitalia)
- Xtra-Anatomy
- Sem 3 (Cardio-Respiratory)
- Sem 4 (Mind & Movement)
- Sem 5 (Body Metabolism)
- Sem 1 (Foundation)
- Posting (Elective)
- Society
- The Insider










