L3- Pharmacological of Antituberculosis
Tuberculosis
-Tuberculosis (TB) remains the leading cause of death worldwide from a single infectious disease agent. Indeed up to 1/2 of the world’s population is infected with TB.
-The registered number of new cases of TB worldwide roughly correlates with economic conditions: the highest incidences are seen in those countries of Africa, Asia, and Latin America with the lowest gross national products.
-WHO estimates that eight million people get TB every year, of whom 95% live in developing countries. An estimated 2 million people die from TB every year
-It is estimated that between 2000 and 2020, nearly one billion people will be newly infected, 200 million people will get sick, and 35 million will die from TB – if control is not further strengthened.
-The mechanisms, pathogenesis, and prophylaxis knowledge is minimal.
-After a century of decline TB is increasing and there are strains emerging which are resistant to antibiotics.
-This excess of cases is attributable to
- the changes in the social structure in cities,
- the human immunodeficiency virus epidemic ,
- the failure of most cities to improve public health programs,
- the economic cost of treating
-TB is an ancient infectious disease caused by Mycobacterium tuberculosis. It has been known since 1000 B.C., so it not a new disease. Since TB is a disease of respiratory transmission, optimal conditions for transmission include:
- overcrowding
- poor personal hygiene
- poor public hygiene
-With the increased incidence of AIDS, TB has become more a problem in the U.S., and the world.
-It is currently estimated that 1/2 of the world’s population (3.1 billion) is infected with Mycobacterium tuberculosis. Mycobacterium avium complex is associated with AIDS related TB.
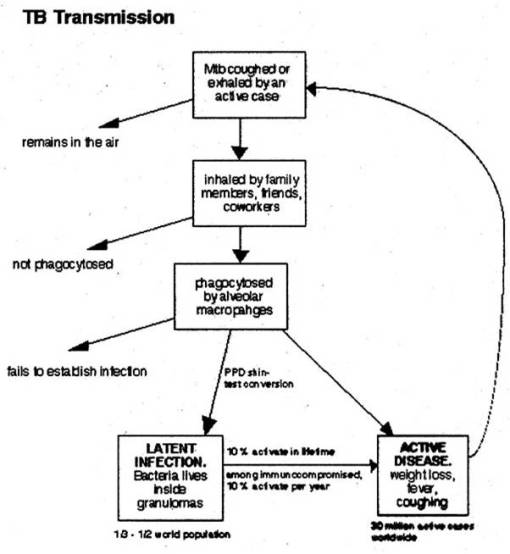
Transmission
-Pulmonary tuberculosis is a disease of respiratory transmission, Patients with the active disease (bacilli) expel them into the air by:
- coughing,
- sneezing,
- shouting,
- or any other way that will expel bacilli into the air
-Once inhaled by a tuberculin free person, the bacilli multiply 4 -6 weeks and spreads throughout the body.
-The bacilli implant in areas of high partial pressure of oxygen:
- lung
- renal cortex
- reticuloendothelial system
-This is known as the primary infection.
-The patient will heal and a scar will appear in the infected loci.
-There will also be a few viable bacilli/spores may remain in these areas (particularly in the lung).
-The bacteria at this time goes into a dormant state, as long as the person’s immune system remains active and functions normally, this person isn’t bothered by the dormant bacillus.
-When a person’s immune system is depressed., a secondary reactivation occurs.
-85-90% of the cases seen which are of secondary reactivation type occurs in the lungs.
Mycobacterium tuberculosis
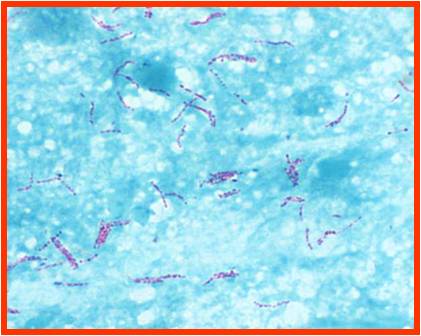
-gram +ve bacilli
-Non motile, non sporing,& noncapsulated
-Strict aerobes
-Branching filamentous forms ≈ fungal mycelium =MYCOBACTERIUM
-A.F.B = when stained by Carbol Fuschin by Z-N Stain they resist decolorisation by 25% H2S04 & Abs.alcohol
-Cell wall is lipid rich with mycolic acid which is essential & unique component


Classification of Drugs
-3 Groups depending upon the degree of effectiveness and potential side effects
First Line: (Primary agents)
-are the most effective and have lowest toxicity.
-Isoniazid Rifampin
Second Line:
-Less effective and more toxic effects
-include (in no particular order): amino salicylic acid, Streptomycin, Ethambutol
Third Line
-are least effective and most toxic.
-Amikacin, Kanamycin, Capreomycin, Viomycin, Kanamycin, Cycloserine


