L2-Physio of Hemostasis (Blood Clot)

Hemostasis
Definition
Stop of blood loss after blood vessel injury.
A series of changes occur to stop blood loss including:
A- Vascular spasm
B-Formation of a platelet plug
C-Formation of a blood clot
1- Vascular spasm
It occurs immediately after blood vessel injury
Mechanism:
Nervous reflexes
Local myogenic contraction
Release of chemical substances
Importance of vascular spasm
1-It reduces blood loss from the ruptured vessels.
2- If the injured blood vessel is very small it can stop bleeding completely.
2- Platelet plug formation
Platelets form a mechanical plug to seal the vascular injury.
– If the injury is small, it can stop bleeding.
– If the injury is large, a blood clot is needed.
Mechanism of platelet plug
a-adhesion
Adhesion of platelets to the exposed subendothelial collagen.
b-activation
Adhesion of platelets initiates platelet activation. Platelets swell, develop pseudopodia and become sticky and secrete their granules mainly ADP and thromboxane A2.
c-aggregation
ADP and Thromboxane A2 activate the nearby platelets making them more sticky and adhere to the already adhered platelets.
d-plug formation

Physiological significance
1-If the damage is small the plug can stop bleeding.
2-Extremely important in closing the minute ruptures that occur thousands daily.
3-It does not occlude the circulation.
Clinical applications
Salicylates (aspirin) can inhibit the thromboxane-A2 and so is used commonly as antiplatelet drug.
3- Blood clot formation
– Within 4-8 minutes after rupture of a vessel, the entire opening is filled with clot especially if the opening is not too large.
In the blood, a balance between 2 groups of substances:
1-Coagulation factors.
2-Anticoagulation factors
However, the anticoagulation factors predominate under normal conditions
Clotting factors
They are mostly plasma proteins especially beta globulin type.
They are mostly proteolytic enzymes present in the blood in the inactive state.
They are designated by names and roman numerals
Factor I : Fibrinogen
Factor II :Prothrombin
Factor III :Tissue thromboplastin
Factor IV : Calcium ions
Other factors up to factor XIII and other added factors
For a blood clot to occur there must be some change that makes the coagulation factors more potent.
Some substances are released from damaged tissues to activate the clotting factors and to initiate the clotting
Mechanism of blood clot
The clotting process is initiated by active substances from:
a-the traumatized vascular wall.
b-from platelets.
c-from blood proteins adhering to the traumatized wall.

Blood clotting takes place in 3 steps:
1-Formation of prothrombin activator in response to:
-trauma to the blood vessel or
-trauma to the blood itself
2-Conversion of prothrombin into thrombin
3-Precipitation of fibrinogen into fibrin threads.
1) Formation of prothrombin activator
A- the extrinsic pathway
It begins with trauma to the vascular wall and surrounding tissues.
B- The intrinsic pathway
It begins in the blood itself.
The extrinsic pathway
1-Traumatized tissues release tissue thromboplastin or tissue factor. It is composed of:
a-Phospholipids from the membranes of the tissue cells.
b-Lipoprotein that function as proteolytic enzyme.
2- The lipoprotein of tissue thromboplastin activates factor VII then complexes with it.
3- This complex in the presence of calcium and tissue phospholipids activates factor X to factor Xa.
4-Xa + tissue phospholipids + factor V to form the prothrombin activator.
The intrinsic pathway
1- It begins by:
A- trauma to the blood itself.
B- exposure of blood to collagen of traumatized vessel wall.
C- contact of blood with water-wettable surface e.g. test tube.
2- As a result, activation of factor XII and release of platelet phospholipid (PF3).
3- Cascade activation of factors XI and IX.
4- IXa + VIII + platelet phospholipid will activate factor X.
5- Xa + V + Ca + PF3 will give the prothrombin activator.
2) Conversion of prothrombin to thrombin
-Prothrombin is a plasma protein (alpha 2 globulin).
-Its concentration in the plasma is about 15 mg%.
-Prothrombin activator convert prothrombin into thrombin.

3) Conversion of fibrinogen into fibrin
-Thrombin is a proteolytic enzyme that changes fibrinogen into fibrin.
– The fibrin threads form the meshwork of the clot.
– Fibrin stabilizing factor is released from the platelets to strengthen the fibrin meshwork.

Blood clot
It is formed of :
-fibrin threads running in all directions
-and entrapping blood cells, platelets and plasma

Role of calcium in the clotting mechanism
Calcium ions share all steps of clot formation except the first 2 steps in the intrinsic pathways.
Calcium de-ionization of blood helps to prevent its coagulation in labs.
Role of vitamin K in blood clotting
Vitamin K is essential for the formation of factors 1, 2, 7, 10.
Fate of a clot
1-Changed into fibrous tissue within 1-2 weeks.
2-It can be dissolved by the fibrinolytic system
Fibrinolytic system
The plasma contains a plasma protein called plasminogen or profibrinolysin . When it is activated it is changed into plasmin which is a proteolytic enzyme that digests fibrin threads.
Plasminogen activators
1-Tissue plasminogen activators (t-PA).
2-Thrombin and active factor XII.
3-Urokinase.
4-Streptokinase.
Significance of fibrinolysis
1- Reopening of blocked small vessels
2-Prevention of blood clotting in nehrons.
3- liquefies menstrual blood.
4-Used clinically either by injection or via a catheter.
Prevention of blood clotting in the normal vascular system
A-Endothelial surface factors:
1-Its smoothness
2-Presence of glycocalyx
3-Trombodulin and protein-C
B-Blood factors:
1-Antithrombin I
2-Antithrombin III
3-Heparin
Anticoagulants
A- In-Vitro anticoagulants
*Precipitation of blood calcium
*Usage of Unwettable silicone
*Heparin
B- In-Vivo anticoagulants
*Heparin
*Coumarin derivatives
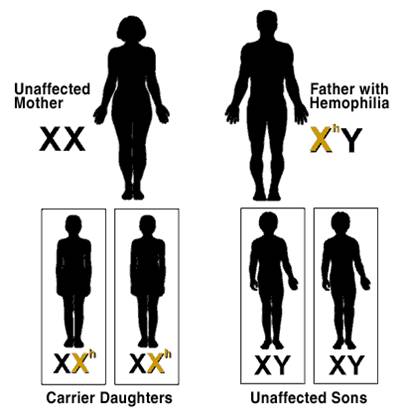
Disorders of hemostasis
A- Conditions of excessive bleeding:
1-Thrombocytopenic purpura
2- Vitamin K deficiency
3- Hemophilia
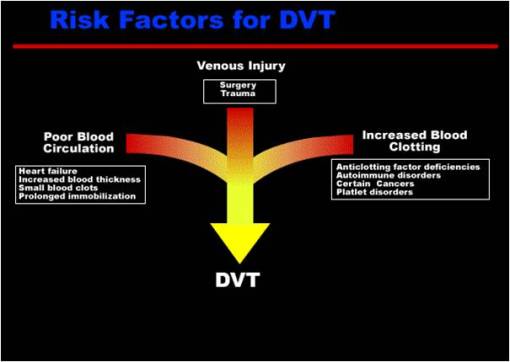
B- Conditions of excessive clot formation:
1- Very slow blood flow
2- Roughness of vascular endothelium
3- Increased blood viscosity e.g. Polycythemia


Deep venous thrombosis

Venous clot formation