Your Medical Frontline
Archive for the ‘ Case 1 (PNX) ’ Category
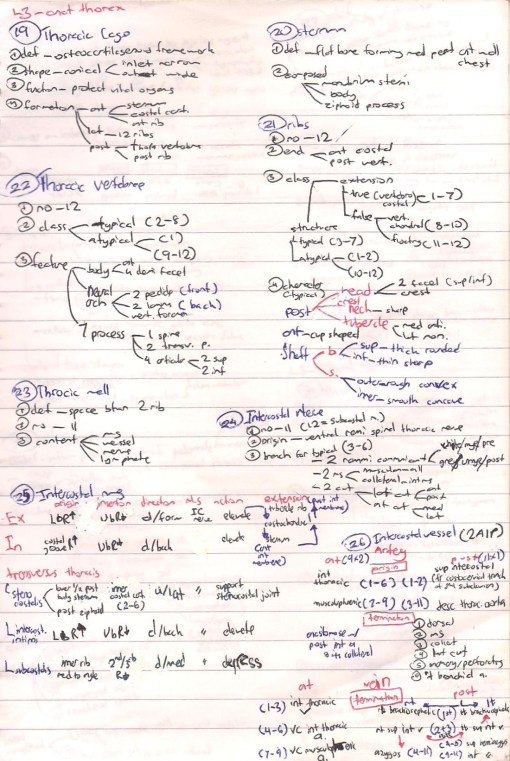
L3- Regulation of Respiration Brain Stem Centre
•The Respiratory system in human performs a critical task
•That is to regulate & respond to O2 demands
•Maintaining a constant O2 & CO2 in the blood
•Therefore, regulation of respiration is critically important for Homeostasis
•Any physiological control system is composed of 3 interconnecting structures:
•Integrator (centre), Sensor & Effector
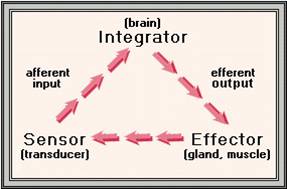
The Respiratory Control System
Integrator (Centre)
→ neural network in brainstem
Sensors
→ The main are chemosensors sensing changes in CO2, O2 & pH
→ Other contributors:
in the lungs, cardiovascular, skeletal muscles, tendons of respiratory muscles
Effector
→ respiratory muscles
Inspiration; diaphragm & external intercostals
Expiration; internal intercostals & abdominal recti
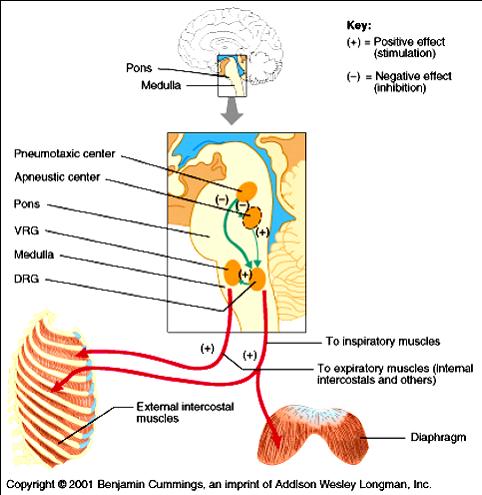
The Respiratory Centre
•Present in brain stem
• 1) Medullary group of neurons (rhythmicty centre)
• 2) Pontine:
- Apneustic
- Pnemotaxic

(I) Medullary Respiratory Neurons (Rhythmicity Centre)
•2 distinct groups of neurons;
- The Dorsal Inspiratory Group (DIG)
- The Ventral Expiratory Group (VEG)
•The 2 groups are bilaterally paired
•There is cross communication between them
- responsible for initiation & regulation of breathing
1 -Dorsal Inspiratory Group (DIG)
•Inspiratory neurons that discharge during inspiration & stop discharging during expiration (Inspiratory Rhythm generator)
•They generate a Ramp Signal;
they initiate inspiration with a weak burst of action potentials that gradually increase in amplitude, then ceases for the next 3 sec until a new cycle begins
•This provides a gradual increase in lung volume during inspiration
Input to DIG
•The most important sensory comes from the adjacent central Chemoreceptors (chemosensitive area in medulla)
•Input from peripheral Chemoreceptors via afferent sensory of vagus (X) & glossopharyngeal (IX)
•Stimulatory input from Apneustic centre prolonging its activity
•Inhibitory input from Pneumotaxic centre terminating its activity
Output from DIG
•Efferent nerves to spinal motoneurons supplying diaphragm (C3-5) & external intercostals (T1-T12).
•Stimulatory to Pneumotaxic centre
2 -Ventral Expiratory Group (VEG)
•Anterolateral to DIG
•Activated during heavy breathing; e.g. exercise
•During such conditions, the increased activity of inspiratory neurons activates the VEG
•In turn, the activated VEG discharge:
- – inhibiting inspiratory group
- – stimulating the muscles of expiration; internal intercostals (T6-L3), abdominal recti (T4-L3)
(II) Pontine Respiratory Centre
•2 pontine centres that modify the rate & The Pattern of respiration
1 -Apneustic centre:
•In the lower 1/3 close to medullary groups
•sends stimulatory discharge to inspiratory neurons promoting inspiration
•Removal of its stimulatory effect→ respiration becomes shallow & irregular

2 -Pneumotaxic centre
•In upper 2/3 of pons
•Its major role is regulation of respiratory volume & rate
•Controlling cessation of inspiratory ramp signal from DIG;
•Switch-off DIG & apneustic centre → expiration occurs
•Hypoactivation of this centre →prolonged deep inspiration with limited brief expiration
•Hyperactivation →shallow inspiration
•Thus the pontine centres work in co-ordination to regulate rhythmic respiratory cycle; How
- Active inspiratory neurones→ ms. of inspiration & pneumotaxic centre → inhibits apneustic & DIG → initiation of expiration
•Spontaneous activity of inspiratory neurons then starts another cycle
(III) The co-ordinated work of neurons of respiratory centre (Pons & Medulla)
Overall Control of Activity of Respiratory Centre
A). Involuntary (Automatic) Control:
- Chemoreceptor Reflexes
- Neurogenic Reflexes
B). Voluntary Control
A). Involuntary Automatic Control
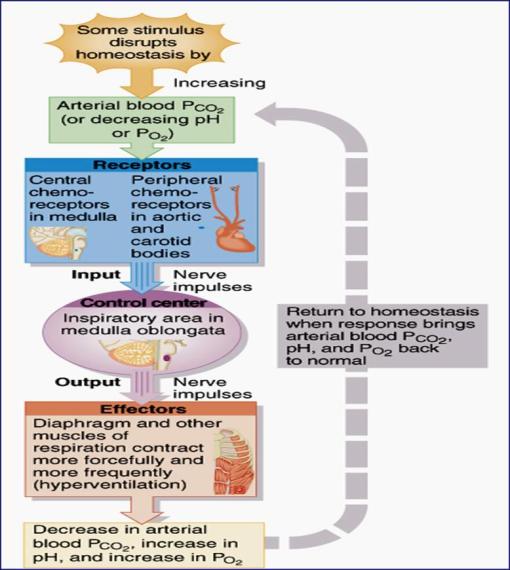
I- Chemoreceptor Reflexes
•Chemical regulation of activity of Respiratory centre which involves 2 pathways:
1- Central Chemoreceptor Pathway
2- Peripheral Chemoreceptor Pathway
•These chemoreceptors sense changes in PCO2, PO2 & pH
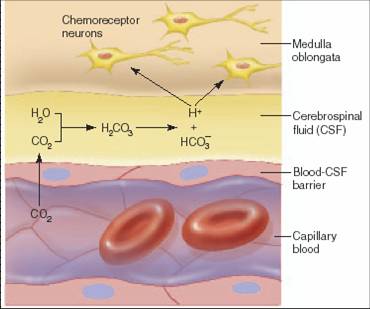
1- Central Chemoreceptors Pathway (Central chemosensitive area)
•Lying just beneath ventral surface of medulla
•Relaying most important sensory input about changes in their close environment to respiratory centre in medulla & pons
•Most sensitive to change in PCO2 ,H+ conc., but not to PO2
 •Under normal conditions, ~75-85% of respiratory drive is due to stimulation of central chemoreceptors by CO2
•Under normal conditions, ~75-85% of respiratory drive is due to stimulation of central chemoreceptors by CO2
•However, central chemoreceptors are directly stimulated only by H+
•But H+ can not cross blood brain barrier while CO2 can
•So, how central chemoreceptors are stimulated by an increase in arterial PCO2?
2- Peripheral Chemoreceptor Pathway (Peripheral Chemoreceptors)
 *Carotid n Aortic Body = Peripheral Chemoreceptors = the only sensors detecting a fall in PO2*
*Carotid n Aortic Body = Peripheral Chemoreceptors = the only sensors detecting a fall in PO2*
Stimulation of Peripheral chemoreceptors
•The carotid & aortic bodies are sensitive to fall in PO2, an increase in PCO2 or H+ concentration
•They maximally stimulated when PO2 decreases below 50-60mm Hg
•They detect changes in dissolved O2 but not in the O2 that is bound to Hb (e.g. in anaemia there is normal PO2 but reduced content of O2 bound to Hb)
 •if there is decreased PO2 (Hypoxia) with absence of peripheral chemoreceptors, Hypoxia will inhibit respiration
•if there is decreased PO2 (Hypoxia) with absence of peripheral chemoreceptors, Hypoxia will inhibit respiration
Why?
•hypoxia depresses neuronal activity including that of respiratory centre
•Hypoxia →VD of cerebral vessels → ↓PCO2 in CSF → ↓CO2-mediated stimulation of central chemoreceptors → hypoventilation
II- Neurogenic Reflexes
- Hering-Breuer Inflation Reflex
- Hering-Breuer Deflation Reflex
- J-receptor Reflex
- Baroreceptors Reflex
- Cough & sneezing Reflexes
- Other influences (mediated via hypothalamus)
1- Hering-Breuer inflation reflex (inhibito-inspiratory reflex)
•Over-Inflation of lungs→ stimulation of slowly adapting stretch receptors in smooth muscles of large & small airways →afferent vagal signals → inhibitory to apneustic centre →termination of inspiration
2- Hering-Breuer deflation reflex (excito-inspiratory reflex)
•Deep expiration → Deflation of the lungs → ↓activity of previous stretch receptors or stimulate other propioceptors in respiratory muscle → vagal afferent signals → inhibition of expiratory neurons
3- J-receptor Reflex
•Pulmonary emboli or oedema →juxtapulmonary-capillaries receptors →vagal afferent to respiratory centre → rapid shallow respiration
•These receptors are responsible for the sensation of air hunger (Dyspnea; shortness of breath)
4- Baroreceptor Reflex
•↑in ABP → stimulation of baroreceptors →afferent signals via X & IX → inhibitory to respiratory centre → decrease rate & depth of respiration → ↓venous return → ↓COP → ↓ABP
5- Cough, Sneezing reflexes
•Dust, smoking, irritant substances → stimulation of irritant receptors in upper airways →afferent signals via vagus (Upper airways, {larynx, cough}) or trigeminal or olfactory (nose, sneezing) → respiratory centre → deep inspiration followed by forced expiration against closed glottis →opening of glottis →forceful outflow of air

6- Other Influences from higher centres hypothalamus & limbic system
•Temperature: Increases respiratory rate
•Pain: Sudden pain decreases, prolonged pain increases rate
•Alcohol: Decreases rate
B). Voluntary Control of Breathing
Cortical Influence
•Through descending tracts from the cerebral cortex to motor neurons of the respiratory muscles (dorsolateral corticospinal tracts)
•This provides CNS the ability to override the automatic regulation of respiration for short time e.g. holding breath but the involuntary control will take over (↑ PCO2, H+), or deliberate hyperventilation (↓PCO2)
Summary in Figures
1) Summary of the Effect of ↑arterial PCO2 on ventilation

2) Effect of a decreased arterial PO2

3) Summary of Chemical Pathways stimulating Ventilation
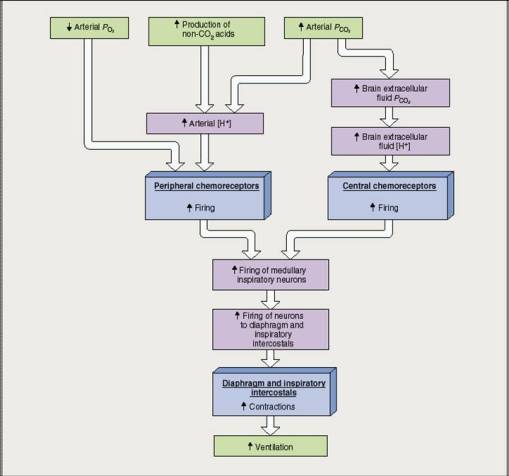
4) Summary Of the Overall Control of Activity of Respiratory Centre

L2-Mechanisms of Respiration
ANATOMY OF RESPIRATORY SYSTEM
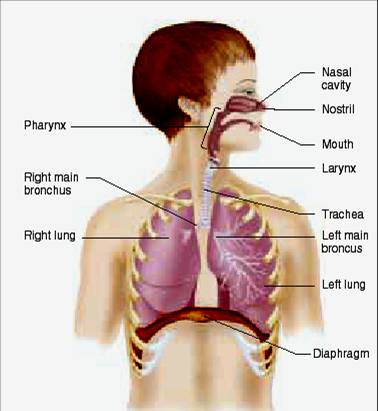
COMPONENT OF RESPIRATORY SYSTEM
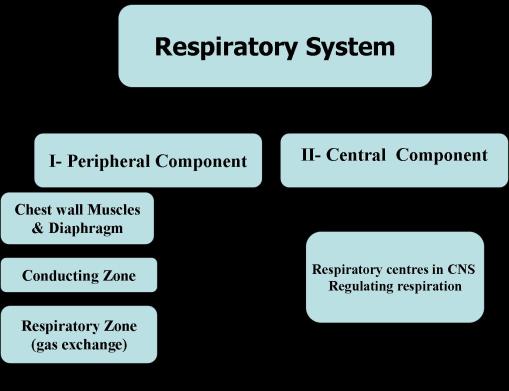
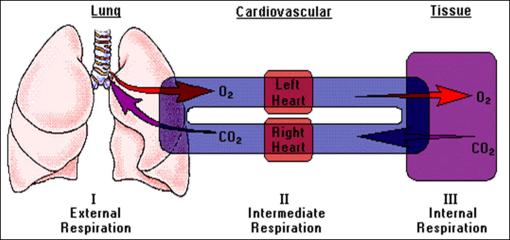
The Main function of the Respiratory system
The Primary function is to obtain oxygen for use by the body’s cells and eliminate CO2 that cells produce.
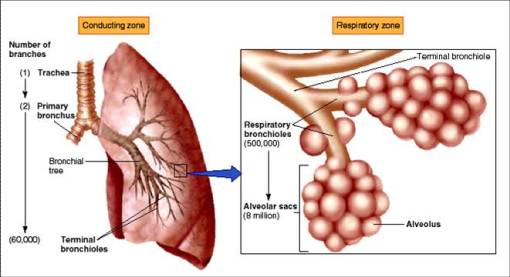
MECHANISMS OF BREATHING
For pulmonary ventilation to occur there should be a pressure gradient driving air in & out
- The movement of air into & out of the lungs (ventilation) occurs as a result of pressure difference between the alveoli & environment
- The pressure differences in pulmonary system are induced by changes in lung volumes occurring as a result of coordinated movement of diaphragm & ches
- The lung volumes are affected by its physical properties; compliance, elasticity & surface tension
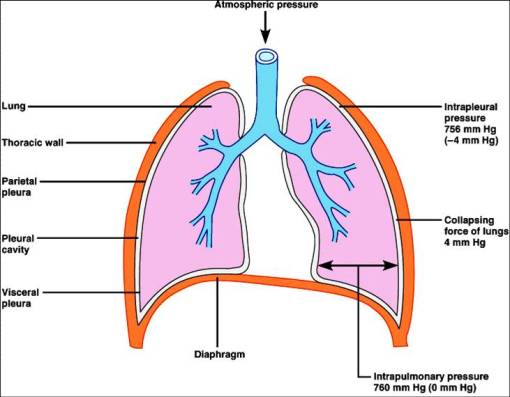
Rest pressures within thoracic cavity
- Atmospheric pressure surrounding the body =760 mm Hg
- Intraalveolar or intrapulmonary pressure: pressure within alveoli =o=atmospheric during rest
- Intrapleural pressure: pressure within pleural sac=subatmospheric= always negative
 Boyle’s Law
Boyle’s Law
•Describing the relationship between volume of gases and its pressure stating that:
P1xV1=P2XV2
•So within a chamber, as the volume of the chamber is increased the pressure of the gas within it decreases & vice versa
So as the volume of chest & lungs change during breathing this leads to change in pressure within the lungs leading to movement of air in & out
Breathing Cycle
-Normal adult breathes about 12-16 breaths or cycles/min
-Breathing cycle (3.7 sec) includes 2 phases followed by a pause:
- Inspiration; the flow of air from atmosphere into the lungs
- Expiration; the flow of air from lungs to outside
- Expiratory pause
Mechanism of Inspiration
Normal Quiet inspiration
-is an active process; caused by contraction of the diaphragm & external intercostal muscles
- The Diaphragm is the main muscle of inspiration (75% of inspiratory act) → increase in the vertical diameter of thoracic cavity
- External intercostal muscles contraction → increase in the lateral dimensions of thoracic cavity

Forced Inspiration
•Forced inspiration is aided by accessory muscles of inspiration;
- sternomastoid (elevation of the sternum)
- scalene muscles (elevation of upper ribs)

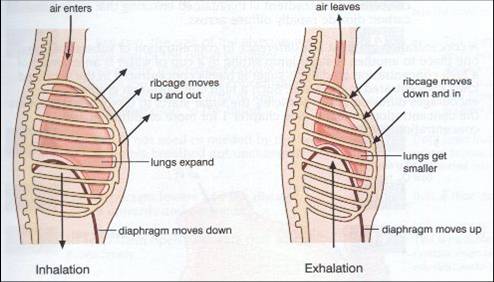
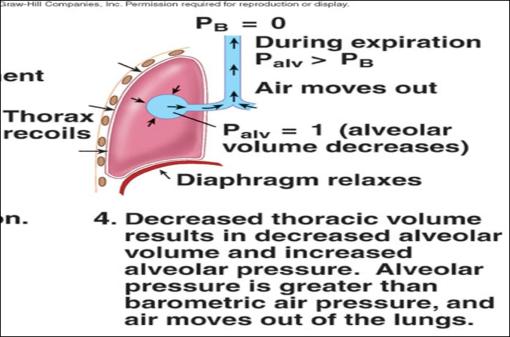
Mechanism of Expiration
Normal Quiet expiration
is a passive process occurring as a result of:
- relaxation of muscles of inspiration
- Elastic recoil of the lungs
- Descent of thoracic cage by gravity
•Leading to decrease in volume of the lungs → increase in intrapulmonary pressure to be greater than atmospheric pressure (+1mm Hg) → pressure gradient → rush of air out of the lungs
Forced expiration
is an active process caused by contraction of muscles of forced expiration;
- abdominal muscles
- internal intercostal muscles
•Contraction of these muscles leads to greater decrease in lung volume and hence greater pressure gradient between intrapulmonary & atmospheric P leading to more air moving out of the lungs
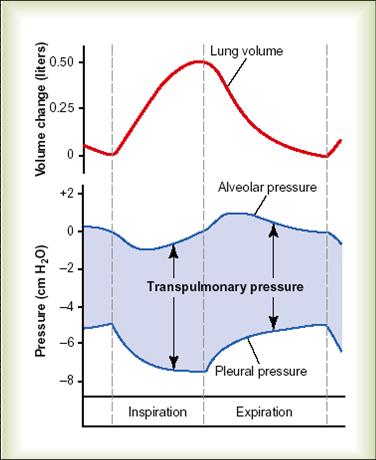
Pressure Relationship during Breathing Cycle

1) Intrapleural pressure (Intrathoracic pressure)
-It is the pressure within the pleural cavity.
-It is always negative which acts as a suction to keep the lungs inflated.

-etiology of the negativity of the intrapleural cavity
- Surface tension of alveolar fluid
- Elasticity of lungs
- Elasticity of thoracic wall
- Minimal volume of air & fluid in pleural cavity
-changes of intrapleural pressure during Eupnoea
- As the thoracic wall moves outward during inspiration, the intrapleural pressure becomes more negative.
- As the thoracic wall recoils during expiration, the pressure returns to normal (756 mmHg)
-IPP values
- -4 mm Hg at end of normal expiration.
- -7 mm Hg at end of normal inspiration.
- -3o mm Hg during forced inspiration
- +30 mm Hg during forced expiration
-Significance of negativity if IPP
1-It helps expansion of the lungs.
2-It helps also:
a-Venous return to the heart
b-Lymphatic drainage
c-Pulmonary blood flow in the pulmonary vessels.
FACTORS OF NORMAL RESPIRATION
1) Elastic recoil of the lungs
•It is the tendency of the lung to return to its original volume when stretched
•Contributes to occurrence of expiration & to negativity of IP
•Due to:
1- elastic fibres; elastin + collagen fibres (responsible for 1/3 of recoil)
2- surface tension of fluid lining alveoli (responsible for 2/3 of recoil)
•This tendency to recoil (tendency to resist distension) is reduced by presence of Surfactant
2) The lung surfactant

•It is a lipoprotein substance secreted by alveolar epithelium into the alveoli.
•It decreases the surface tension of the fluid lining the alveoli
•It is secreted among the fluid molecules, so decreasing the attraction between them and lowering the surface tension
•physiological significance of surfactant
- Prevention of collapse of small alveoli especially during expiration.
- Decrease of muscular effort needed to ventilate the lungs.
- It has an immune effect to protect the lugs against invaders
•surfactant decreases in the following conditions
1-Respiratory distress syndrome (hyaline membrane disease)
2-Cigarette smoking.
3-After cardiac surgery.
4-Elective cesarean section
3) Compliance
•Compliance is a measure of the ease of inflation of the lungs (measure of distensibility)
•Measured as the change in lung volume for a certain change in transpulmonary pressure (alveolar P-IPP) ; C= ΔV/ ΔP
•When a small change in pressure causes a large change in volume, this is expressed as a highly compliant lung
•Lung compliance =200 ml/ 1cm H2O pressure
•Lung + chest compliance = 130 ml/cm H2O
•Factors affecting Compliance
1) Factors in the lungs:
- Conditions ↑ surface tension → ↑elastic recoil of the lung (decreasing lung expansion) →↓ complianc
- Conditions ↓ elastic tissues of lung as in lung fibrosis → ↓compliance
2) Factors in the chest;
Compliance is decreased by
- Chest deformities
- Bone diseases
- Muscle diseases
- Obesity
COMPLICATION DUE RESPIRATORY IMPAIRMENT
Pneumothorax
-It is the collapse of the lung due to a puncture into the pleural cavity of chest wall or the lungs.
-The collapse results from air entering the pleural cavity, as it moves from high pressure to low pressure.
-If one lung is punctured, the other lung is unaffected.
This is because the lungs are completely separate from one another.
Each lung is surrounded by its own pleural cavity and pleural membrane. Therefore, changes in the intrapleural pressure of one lung is independent of the other lung.

-Types of pneumothorax
1-Closed:
When there is a small hole in the thoracic wall or the lung (spontaneous). The air will be gradually absorbed and the IPP returns negative
2-Open:
When the hole is large. The IPP is atmospheric.
3-Valvular (Tension):
When a flap of tissue over the hole acts as a valve that allows air entry during inspiration but prevents its escape during expiration. The IPP is positive and the lung is severely collapsed.
L1-Thoracic Wall
OBJECTIVE
1) Thoracic Cage
Surface Marking
2) Intercostal Spaces
3) Diaphragm
4) Pleura
5) Surface Anatomy
[1] THORACIC CAGE
- the ribs and intercostal spaces on each side
- the sternum and costal cartilage in front
- the vertebral column behind
- above; the THORACIC INLET communicates with root of the neck
- below; the THORACIC OUTLET separated from the abdominal cavity by diaphragm

TYPICAL RIBS
- curved
- Posterior End
- Head
- Tubercle
- Anterior End
- Costal Groove
- articulate with 2 vertebrae
- the synovial joint permits up and down rib movements

SURFACE MARKING
- sternum (3 parts)
- jugular notch
- sternal angle
- clavicle
- costal margin
- infrasternal angle
- midclavicular line
- midaxillary line

[2] INTERCOSTAL SPACE
DEFINITION: It is the space between 2 ribs
NUMBER: 11
CONTENTS:
- Intercostal Muscles
- Intercostal Vessels
- Intercostal Nerves
- Lymphatics
→INTERCOSTAL MUSCLES
1) THE EXTERNAL INTERCOSTAL MUSCLE
- its fiber pass forwards
- extend from tubercle of ribs to costocartilage junctions
- continues as EXTERNAL INTERCOSTAL MEMBRANE
- elevate the ribs during inspiration
ORIGIN:
-Lower border of rib above
INSERTION:
-Upper border of rib below
DIRECTION OF FIBERS:
-Downward and Forward
EXTENT:
-From the tubercle of rib (behind) to the costochondral junction (in front) where it continues as a membrane (ANTERIOR @ EXTERNAL INTERCOSTAL MEMBRANE)
NERVE SUPPLY:
-Intercostal Nerves
ACTION:
Elevation of ribs during inspiration

2) THE INTERNAL INTERCOSTAL MUSCLE
- its fibers pass backwards
- extends from edge of sternum to angle of the rib
- continues as INTERNAL INTERCOSTAL MEMBRANE
- depress ribs in expiration
ORIGIN:
-Costal groove of rib above
INSERTION:
-Upper border of tib below
DIRECTION OF FIBERS:
-Downward and Backward
EXTENT:
-From lateral margin of sternum (anteriorly) to the angle of rib (posteriorly) where it continues as a membrane (POSTERIOR @ INTERNAL INTERCOSTAL MEMBRANE)
NERVE SUPPLY:
-Intercostal Nerve
ACTION:
-Elevation of ribs during expiration

3) TRANSVERSUS THORACIC MUSCLE
- is separated from intenal intercostal muscle by the NEUROVASCULAR BUNDLE
- the fibers of this sheet cross more than one space
- Subcostalis
- Intercostalis Intimi (Innermost Intercostal)
- Sternocostalis
1- STERNOCOSTALIS MUSCLE
ORIGIN:
-Lower 1/3 posterior surface of body of sternum & xiphoid process
INSERTION:
-Costal cartilages from 2nd to 6th
DIRECTION OF FIBERS:
-Upward and laterally
NERVE SUPPLY:
-Intercostal Nerve
ACTION:
-Support the sternocostal joint
2- INTERCOSTALIS INTIMI MUSCLE
ORIGIN:
-Lower border of rib above
INSERTION:
-Upper border of rib below
DIRECTION OF FIBERS:
-Downwards and Backward (as inner intercostal ms)
-Along the mid 2/4 of intercostal space
NERVE SUPPLY:
-Intercostal Nerves
ACTION:
-Elevation of ribs during inspiration
3- SUBSCOSTALIS MUSCLE
ORIGIN:
-Slips from the inner surface of rib at its angle
INSERTION:
-The 2nd or 3rd rib below
DIRECTION OF FIBERS:
-Downward and Medially
NERVE SUPPLY:
-Intercostal nerve
ACTION:
-Depress the ribs during expiration


→INTERCOSTAL VESSELS AND NERVES
- VAN (vein , artery , nerve)
- lie in subcostal groove
- between Internal Intercostal and Innermost Intercostal Muscle

ARTERIES
1) ANTERIOR INTERCOSTAL ARTERIES
NO:
-TWO in each space (9 spaces) = 18
BEGINNING:
-upper 6 from INTERNAL THORACIC ARTERY
-lower 3 from MUSCULOPHRENIC ARTERY (branch of Internal Thoracic Artery)
TERMINATION:
-by anastomosing with POSTERIOR INTERCOSTAL ARTERIES & their collateral branches
COURSE:
-pass laterally in the intercostal space

(1) – Internal Thoracic @ Mammary Artery
(2) – Supreme Thoracic Artery(branch of axillary a.)
(3) – Lateral Thoracic Artery
(4) – Intercostal Artery
2) POSTERIOR INTERCOSTAL ARTERIES
NO:
-one in each space (11 spaces) = 11
BEGINNING:
-upper 2 from sup intercostal artery branch of costocervical trunk of 2ND part SUBCLAVIAN ARTERY
-lower 9 from branches of descending THORACIC AORTA
TERMINATION:
-ends near the costochondral junction by anastomosing with CORRESPONDING ANTERIOR INTERCOSTAL ARTERY
BRANCHES:
1)DORSAL B.
-arise at neck of rib
-supplies muscle and skin of back and the spinal cord & its meninges
2)COLLATERAL BRANCH
-arises near the angle of rib
-runs along the upper border of rib below
-terminates by anastomosing w/ ANT INTERCOSTAL A.
3)LATERAL CUTANEOUS B.
-arises near angle of rib
-accompanies the lateral cutaneous branch of intercostal nerve
4)MAMMARY B.
-arises from 2nd , 3rd , 4th POST INTERCOSTAL A.
-supplies the lateral parts of the mammary gland(breast)
5)MUSCULAR B.
-to the surrounding muscles
6)RIGHT BRONCHIAL ARTERY
-from right third POST INTERCOSTAL A.

3) INTERNAL THORACIC (MAMMARY ARTERY)
ORIGIN:
-first part of SUBCLAVIAN A.
TERMINATION:
-opposite 6th intercostal space by dividing into
- SUPERIOR EPIGASTRIC ARTERY
- MUSCULOPHRENIC ARTERY
COURSE & RELATIONS:
-descend downward and medially
-behind clavicle and 1st costal cartilage
-descend vertically downward to termination @ 6th i. space
BRANCHES:
1)PERICARDIOPHRENIC A.
-runs w/ phrenic nerve
-supplies pericardium, pleura, diaphragm
2)ANTERIOR INTERCOSTAL A.
-two for each space(6 spaces)
3)PERFORATING A.
-accompany anterior cutaneous nerve and the perforating branches of 2nd, 3rd, and 4th spaces supplying mamary gland
4)MUSCULOPHRENIC A
5)SUPERIOR EPIGASTRIC A.
(1)-Internal Thoracic or Mammary Artery
VEIN
1) INTERNAL THORACIC VEIN
BEGINNING:
-behind 3rd costal cartilage by union of vena commitants of INTERNAL MAMMARY ARTERY (which is the result of union of vena commitants of SUP EPIGASTRIC & MUSCULOPHRENIC A.)
TERMINATION:
-in corresponding brachiocephalic vein
TRIBUTARIES:
-corresponding to the branches of INTERNAL THORACIC A.
2) ANTERIOR INTERCOSTAL V.
-drain into INTERNAL THORACIC V.
3) POSTERIOR INTERCOSTAL V.
-drain into the AZYGOS system of veins
4) LEFT SUPERIOR INTERCOSTAL V.
-drain into LEFT BRACHIOCEPHALIC V

NERVE
INTERCOSTAL NERVES
DEFINITION:
-Ventral rami of thoracic spinal nerves in corresponding intercostal space.
-The last thoracic nerve (12th) called SUBCOSTAL NERVE
NO:
-11 intercostal nerves pass in the corresponding intercostal spaces
TYPES:
1) TYPICAL INTERCOSTAL NERVE
-from 3rd to 6th (only at chest wall only)
2) ATYPICAL INTERCOSTAL NERVE
-upper 2 and last 5 (outside chest wall)
1) TYPICAL INTERCOSTAL NERVES
NO:
-from 3rd to 6th i-spaces
BEGINNING:
-exit from corresponding intervertebral foramen from 3rd to 6th intercostal nerves
TERMINATION:
-between Internal I-C Ms and Ant I-C Membrane
-as Anterior Cutaneous Nerve
COURSE & RELATIONS:
1) exits from the corresponding intervertebral foramen
2) pass btwn parietal pleura and post intercostal membrane
3) at angle of ribs, it split the internal intercostal muscle into internal intercostal muscle (outer layer) and innermost intercostal muscle (inner layer)
4) enter costal groove where it lies below the posterior intercostal vessels (V.A.N)
5) at costochondral junctions,it comes out from internal intercostal muscle and runs btwn it and pleura
6) about 1 cm lateral to the sternum, the nerve pierce the internal intercostal muscle and anterior intercostal membrane, to terminate as ANTERIOR CUTANEOUS NERVE
BRANCHES:
1)GANGLIONIC B.
-it give a white myelinated (preganglionic) ramus communicant to the sympathetic trunk and receive a gray unmyelinated (postganglionic) ramus communicant from the correponding ganglion of sympathetic trunk
2)MUSCULAR B.
-to supply intercostal muscles
3)COLLATERAL B.
-runs along the upper border of rib below
4)LATERAL CUTANEOUS B.
-arises close to the angle of rib and pierce the internal and external intercostal muscles
-supply skin at side of chest
5)ANTERIOR CUTANEOUS B.
-is the termination of the intercostal nerve
-supply the skin on front of chest

2) ATYPICAL INTERCOSTAL NERVES
BRANCHES
1)THE 1ST INTERCOSTAL NERVE
-it is atypical because
only small part of it forms the 1st intercostal nerve
but the larger part ascend in front of neck of 1 st rib to share in formation of brachial plexus of upper limb
2)THE 2ND INTERCOSTAL NERVE
-it is atypical because
it supplies the skin of axilla and the arm by its lateral cutaneous branch, which enters the arm as intercostobrachial nerve
3)THE LOWER 5 INTERCOSTAL NERVES
-they are atypical because
their complete courses are in the abdomen

My Blog My Rule
Blog Stats
- 322,266 hits
| S | M | T | W | T | F | S |
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |||
| 5 | 6 | 7 | 8 | 9 | 10 | 11 |
| 12 | 13 | 14 | 15 | 16 | 17 | 18 |
| 19 | 20 | 21 | 22 | 23 | 24 | 25 |
| 26 | 27 | 28 | 29 | 30 | 31 | |
Mansoura Manchester Medical Programme
- Islam
- Fiqh
- Global Issues
- Hadith
- Kitab
- Palestinaku
- Pra-Muraqazah
- Sautun Nahdhah (Suara Kebangkitan)
- SN001 – 28 Rejab Hari Kejatuhan Khilafah
- SN002 – Susah Sangatkah Untuk Bersatu
- SN003 – Buang Bayi – Natijah Dari Dibuangnya Hukum ALLAH!
- SN004 – YA ALLAH! Demi Ramadhan Yang Mulia Ini, ENGKAU Hancurkanlah Pemimpin Yang Jahat Dan Berilah Kemenangan Kepada Pejuang Agamamu
- SN005 – Tanpa Khilafah,Islam Terus Dihina
- SN006 – Nyawa Hilang Nilai Hasil Penolakan Sistem Islam
- SN007 – Halatuju Politik Baru, Menghala Ke Mana?
- SN008 – Islamic Fashion Festival (IFF) Menghina Islam!
- SN009- Mahukah Anda Berzina Dengan Ibu Sendiri?
- SN010 – Amerika Ditatang,Islam Ditentang!
- SN011 – PILIHANRAYA : Sampai Bila Akan Menjadi Topeng Demokrasi
- SN012 – Hijrah Rasullullah Adalah Keluar Dari Darul Kufur Menuju Darul Islam
- SN013 – WIKILEAKS: Antara Bukti Kejahatan Pemimpin Dan Tajassus
- SN014 – Cabaran Dan Tentangan Sejurus Berdirinya Khilafah
- SN015 – Muhasabah Terhadap Harakah Islam Yang Mengakui Sistem Taghut
- SN016 – Tunisia Perlukan Khilafah, Bukan Sekadar Pertukaran Pemimpin
- SN017 – Mesir Bangkitlah Menuju Perubahan Hakiki Dengan Khilafah
- SN018 – Seruan Hizbut Tahrir Kepada Majlis Tertinggi Angkatan
- SN019 – Mempersiapkan Suasana Thalabun Nusrah Untuk Meraih Kekuasaan
- SN020 – Arab Saudi Dan Pengkhianatan Keluarga Saud
- SN021 – Kekejaman Diktator Libya & Keengganan Para Penguasa Kaum Muslimin Menolong Libya
- Sirah
- Tazkirah
- Tokoh2 Islam
- MMMP
- Sem 1 (Foundation)
- Case 1 (Chem of Life)
- Case 2 (Cell Structure)
- Case 3 (Active & Passive Movement)
- Case 4 (Transcription @ Translation)
- Case 5 (Vitamins,Fat & Water)
- Case 6 (Digestion & Absorption)
- Case 7 (Changes in Electrical Activity Caused by Damage)
- Case 8 (Lung Function,Environment & Epidemiology)
- Case 9 (Inherited Disease)
- Case Ten (Chemistry of Sugar)
- Pract/Osce
- Unseen Case (How's The Body is Regulated)
- Sem 2 (Life Cycle)
- Case 01 (Normal Pregnancy)
- Case 02 (Congenital Heart Disease)
- Case 03 (Thalassemia)
- Case 04 (Hypogonadism)
- Case 05 (Immunodeficiency-HIV/AIDS)
- Case 06 (Autoimmune-SLE)
- Case 07 (Autoimmune-Rheumatoid Arthritis)
- Case 08 (Breast Cancer)
- Case 09 (Osteoporosis)
- Case 10 (Menopause)
- Unseen Case (Ambiguous Genitalia)
- Xtra-Anatomy
- Sem 3 (Cardio-Respiratory)
- Sem 4 (Mind & Movement)
- Sem 5 (Body Metabolism)
- Sem 1 (Foundation)
- Posting (Elective)
- Society
- The Insider