Your Medical Frontline
Archive for the ‘ Case 8 (CHD/IHD) ’ Category
L2-Physio of Hemostasis (Blood Clot)

Hemostasis
Definition
Stop of blood loss after blood vessel injury.
A series of changes occur to stop blood loss including:
A- Vascular spasm
B-Formation of a platelet plug
C-Formation of a blood clot
1- Vascular spasm
It occurs immediately after blood vessel injury
Mechanism:
Nervous reflexes
Local myogenic contraction
Release of chemical substances
Importance of vascular spasm
1-It reduces blood loss from the ruptured vessels.
2- If the injured blood vessel is very small it can stop bleeding completely.
2- Platelet plug formation
Platelets form a mechanical plug to seal the vascular injury.
– If the injury is small, it can stop bleeding.
– If the injury is large, a blood clot is needed.
Mechanism of platelet plug
a-adhesion
Adhesion of platelets to the exposed subendothelial collagen.
b-activation
Adhesion of platelets initiates platelet activation. Platelets swell, develop pseudopodia and become sticky and secrete their granules mainly ADP and thromboxane A2.
c-aggregation
ADP and Thromboxane A2 activate the nearby platelets making them more sticky and adhere to the already adhered platelets.
d-plug formation

Physiological significance
1-If the damage is small the plug can stop bleeding.
2-Extremely important in closing the minute ruptures that occur thousands daily.
3-It does not occlude the circulation.
Clinical applications
Salicylates (aspirin) can inhibit the thromboxane-A2 and so is used commonly as antiplatelet drug.
3- Blood clot formation
– Within 4-8 minutes after rupture of a vessel, the entire opening is filled with clot especially if the opening is not too large.
In the blood, a balance between 2 groups of substances:
1-Coagulation factors.
2-Anticoagulation factors
However, the anticoagulation factors predominate under normal conditions
Clotting factors
They are mostly plasma proteins especially beta globulin type.
They are mostly proteolytic enzymes present in the blood in the inactive state.
They are designated by names and roman numerals
Factor I : Fibrinogen
Factor II :Prothrombin
Factor III :Tissue thromboplastin
Factor IV : Calcium ions
Other factors up to factor XIII and other added factors
For a blood clot to occur there must be some change that makes the coagulation factors more potent.
Some substances are released from damaged tissues to activate the clotting factors and to initiate the clotting
Mechanism of blood clot
The clotting process is initiated by active substances from:
a-the traumatized vascular wall.
b-from platelets.
c-from blood proteins adhering to the traumatized wall.

Blood clotting takes place in 3 steps:
1-Formation of prothrombin activator in response to:
-trauma to the blood vessel or
-trauma to the blood itself
2-Conversion of prothrombin into thrombin
3-Precipitation of fibrinogen into fibrin threads.
1) Formation of prothrombin activator
A- the extrinsic pathway
It begins with trauma to the vascular wall and surrounding tissues.
B- The intrinsic pathway
It begins in the blood itself.
The extrinsic pathway
1-Traumatized tissues release tissue thromboplastin or tissue factor. It is composed of:
a-Phospholipids from the membranes of the tissue cells.
b-Lipoprotein that function as proteolytic enzyme.
2- The lipoprotein of tissue thromboplastin activates factor VII then complexes with it.
3- This complex in the presence of calcium and tissue phospholipids activates factor X to factor Xa.
4-Xa + tissue phospholipids + factor V to form the prothrombin activator.
The intrinsic pathway
1- It begins by:
A- trauma to the blood itself.
B- exposure of blood to collagen of traumatized vessel wall.
C- contact of blood with water-wettable surface e.g. test tube.
2- As a result, activation of factor XII and release of platelet phospholipid (PF3).
3- Cascade activation of factors XI and IX.
4- IXa + VIII + platelet phospholipid will activate factor X.
5- Xa + V + Ca + PF3 will give the prothrombin activator.
2) Conversion of prothrombin to thrombin
-Prothrombin is a plasma protein (alpha 2 globulin).
-Its concentration in the plasma is about 15 mg%.
-Prothrombin activator convert prothrombin into thrombin.

3) Conversion of fibrinogen into fibrin
-Thrombin is a proteolytic enzyme that changes fibrinogen into fibrin.
– The fibrin threads form the meshwork of the clot.
– Fibrin stabilizing factor is released from the platelets to strengthen the fibrin meshwork.

Blood clot
It is formed of :
-fibrin threads running in all directions
-and entrapping blood cells, platelets and plasma

Role of calcium in the clotting mechanism
Calcium ions share all steps of clot formation except the first 2 steps in the intrinsic pathways.
Calcium de-ionization of blood helps to prevent its coagulation in labs.
Role of vitamin K in blood clotting
Vitamin K is essential for the formation of factors 1, 2, 7, 10.
Fate of a clot
1-Changed into fibrous tissue within 1-2 weeks.
2-It can be dissolved by the fibrinolytic system
Fibrinolytic system
The plasma contains a plasma protein called plasminogen or profibrinolysin . When it is activated it is changed into plasmin which is a proteolytic enzyme that digests fibrin threads.
Plasminogen activators
1-Tissue plasminogen activators (t-PA).
2-Thrombin and active factor XII.
3-Urokinase.
4-Streptokinase.
Significance of fibrinolysis
1- Reopening of blocked small vessels
2-Prevention of blood clotting in nehrons.
3- liquefies menstrual blood.
4-Used clinically either by injection or via a catheter.
Prevention of blood clotting in the normal vascular system
A-Endothelial surface factors:
1-Its smoothness
2-Presence of glycocalyx
3-Trombodulin and protein-C
B-Blood factors:
1-Antithrombin I
2-Antithrombin III
3-Heparin
Anticoagulants
A- In-Vitro anticoagulants
*Precipitation of blood calcium
*Usage of Unwettable silicone
*Heparin
B- In-Vivo anticoagulants
*Heparin
*Coumarin derivatives
Disorders of hemostasis
A- Conditions of excessive bleeding:
1-Thrombocytopenic purpura
2- Vitamin K deficiency
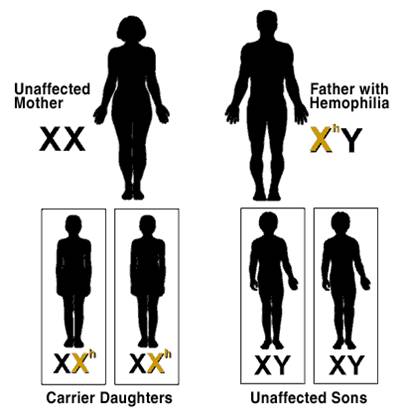
3- Hemophilia
B- Conditions of excessive clot formation:
1- Very slow blood flow
2- Roughness of vascular endothelium
3- Increased blood viscosity e.g. Polycythemia


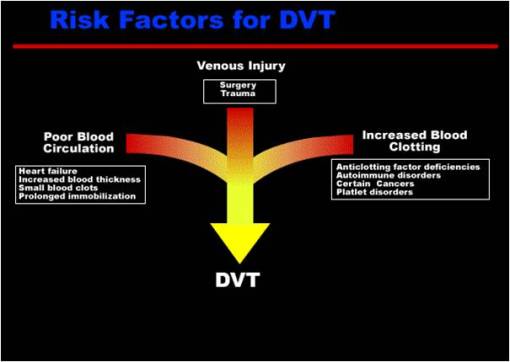
Deep venous thrombosis

Venous clot formation
L3- Pathology of Thrombosis and Embolism

Thrombosis
It is the process of thrombus formation.
Thrombus
-It is a compact mass formed of the circulating blood elements within the cardiovascular system during life.
-Is a solid mass formed of blood elements inside the cardiovascular system during life
Predisposing factors for thrombosis:-
Three main factors (Virchow’s triad)
1- Endothelial damage (dysfunction).
2- Change in the pattern of blood flow (stasis or turbulence).
3- Changes in composition of blood ( blood coagulability).

Thrombus
Is a solid mass formed of blood elements inside the cardiovascular system during life
Predisposing factors for thrombosis:-
1) Endothelial damage (dysfunction)
2) Change in the pattern of blood flow (stasis or turbulence).

3- Changes in composition of blood ( blood coagulability).
Increased concentration of coagulation proteins or reduced concentration of natural anticoagulants. This change may be hereditary ,acquired or immune mediated
A- Hereditary:-
* About 5-10% of all people have some genetic defect predisposing them to thrombosis.
* These include congenital deficiency of antithrombin III, protein C and protein S and mutation in the gene encoding factor V.
B- Acquired :-
* Tissue damage….increase the production of thromboplastin and other procoagulants.
* Chronic infection…. Liver produces excess fibrinogen (one of acute phase reactants).
* Estrogen containing oral contraceptives….increase the production of prothrombin and fibrinogen.
*Tumors…..increased release of thromboplastin.
C- Immune mediated thrombosis
*Heparin-induced thrombocytopenia
-seen in 5% of patients with chronic use of high molecular weight heparin.
– Caused by antibodies to the complex of heparin and platelet factor 4 → Antibodies cross reacts with platelets and endothelial cells → platelet and endothelial injury → thrombosis.
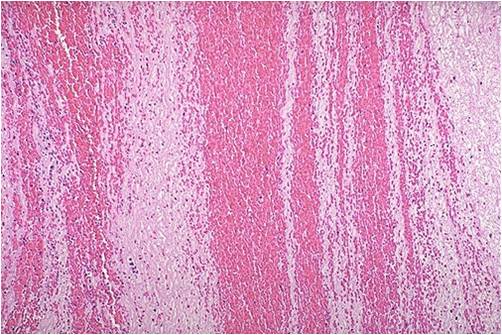
Morphology of thrombi
Large thrombi formed in veins, arteries and heart of living patients have typical features that distinguish them from postmortem clots. These include
1- Lines of Zhan:-
Formed by deposition of platelets and fibrin, which form a white layer. RBCs deposit on this layer forming a red layer on which a new layer of fibrin and platelets is deposited. These alternating white and red lines are called lines of Zhan .

2- Friability :-
Thrombi are held together with fibrin that does not permeate all layers uniformly but leaves cleavage lines between the white and red layers. The friability of thrombi accounts for the fact that they may detach and embolize.
3- Attachment:-
Thrombi are attached to the surface of the vessel or heart chamber in which they arise.
4- Molding :-
Thrombi formed inside veins typically retain the shape of the vessel in which they originate. They fill and expand the affected vessel and its tributaries.
* Postmortem clots
They differ from thrombi in that
1- They form in stagnant (non-circulating) blood.
2- Red blood cells sediment and separate from plasma forming (red current jelly) the plasma above forms a yellow part (chicken fat). No lines of Zhan are formed.
3- They are not attached to the wall of blood vessel and can be washed easily from it.
4- They are soft and moist ( not friable).
5- They do not fill or expand the affected vessel.
Sites of thrombi
Thrombi that occur in different parts of the circulation have different causative factors and different macroscopic appearances

Venous thrombi “phlebothrombosis”
– Form in slow-moving blood.
– Have a high proportion of trapped red cells in relation to platelet/fibrin therefore they are red, soft gelatinous with poor lamination.
– They grow (propagate) towards the direction of the heart.
– They may detach to produce emboli
– Thrombi of infected veins are called thrombophlebitis. They are the source of infected emboli (pyemia).
– Almost all venous thrombi occlude the lumen and prevent blood flow…..Occlusive thrombi.
– Thrombi over cusps of the heart are called vegetations

Leg vein thrombosis
Conditions associated with an increased risk of thrombosis
1- Deep venous thrombosis of LL (DVT) less commonly superficial varicosities.
2- Massive tissue damage e.g. trauma , burns or major surgery are commonly associated with thrombosis. Increased blood coagulability and prolonged bed rest resulting in stasis are responsible factors.
3- Pregnancy and obstetric conditions, prolonged use of oral contraceptives, and steroid therapy.
4- Myocardial infarction, strokes and atherosclerosis.
5- Tumors…release thromboplastin….++ thrombosis.
* Outcome of thrombosis

1-Resolution:-
Fibrinolysis of the thrombus is mediated by plasmin.Since the endothelium lining veins produce more plasminogen activator, venous thrombi are resolved more readily than arterial and cardiac thrombi.
2- Propagation:-
Due to deposition of more platelets, fibrin and RBCs. A tail is formed which is more liable for detachment and embolization.
– Propagation occurs more with venous thrombi and progress towards the direction of the heart.
3- Embolization:
Due to detachment of thrombi from vessel wall.
– Septic thrombi produce pyemia.
4- Organization
Ingrowth of granulation tissue from vessel wall into the thrombus. Later on it changes to fibrous tissue which may be incorporated into the vessel wall.



5- Recanalization
Blood vessels in the granulation tissue may fuse into larger channels that bridge the thrombus with partial restoration of the blood flow in the affected vessel.



Embolism
Definition
It is a detached intravascular solid, liquid or gaseous material that is carried by blood to a site distant from its point of origin to be impacted in a small blood vessel.
Types
1- 99% ..thrombo-embolism
2- Fat emboli
3- Parasitic emboli
4-Air or nitrogen emboli
5- Amniotic fluid emboli
6- Tumor emboli
Clinically most important emboli are:-
1- Venous emboli….originating mostly from thrombi of the leg veins and produce pulmonary embolism.
2- Arterial emboli….originating from the heart, aorta or large vessels and produce systemic embolism e.g. in the brain, kidney and spleen.
1) Pulmonary embolism
In 95% of cases they originate from thrombi of deep leg veins above the level of the knee.
Effects on the lung depend upon the size of the embolus and state of the lung:-
1- 60-80% of cases are small and clinically silent.
2 – 3 size of embolism
Large sized emboli
-obstruct the pulmonary bifurcation (saddle emboli) or one of main pulmonary arteries……sudden death (acute right sided failure) without manifestations of pulmonary infarction.



Medium sized emboli
– with normal lung have no effect why?
– With lung congestion it produce pulmonary infarction.
Small repeated emboli
With time they produce pulmonary hypertension ending in right –sided heart failure (cor-pulmonale)

2) Fat emboli
Causes:-
-Fracture of long bones.
– Trauma or burn to fatty tissue.
Effects :-
– Mechanical obstruction.
– Chemical release of FFA… local toxic effects with injury to vascular endothelium and platelet adhesion.


3) Air embolism
Causes:-
1-Injury of jugular vein.
2- childbirth or abortion.
3- Blood transfusion under positive pressure.
Effects:-
– Small amounts…no effects
– More than 100 cc. → Fill the right side of the heart → acute heart failure → Death.

My Blog My Rule
Blog Stats
- 322,264 hits
| S | M | T | W | T | F | S |
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | |||
| 5 | 6 | 7 | 8 | 9 | 10 | 11 |
| 12 | 13 | 14 | 15 | 16 | 17 | 18 |
| 19 | 20 | 21 | 22 | 23 | 24 | 25 |
| 26 | 27 | 28 | 29 | 30 | 31 | |
Mansoura Manchester Medical Programme
- Islam
- Fiqh
- Global Issues
- Hadith
- Kitab
- Palestinaku
- Pra-Muraqazah
- Sautun Nahdhah (Suara Kebangkitan)
- SN001 – 28 Rejab Hari Kejatuhan Khilafah
- SN002 – Susah Sangatkah Untuk Bersatu
- SN003 – Buang Bayi – Natijah Dari Dibuangnya Hukum ALLAH!
- SN004 – YA ALLAH! Demi Ramadhan Yang Mulia Ini, ENGKAU Hancurkanlah Pemimpin Yang Jahat Dan Berilah Kemenangan Kepada Pejuang Agamamu
- SN005 – Tanpa Khilafah,Islam Terus Dihina
- SN006 – Nyawa Hilang Nilai Hasil Penolakan Sistem Islam
- SN007 – Halatuju Politik Baru, Menghala Ke Mana?
- SN008 – Islamic Fashion Festival (IFF) Menghina Islam!
- SN009- Mahukah Anda Berzina Dengan Ibu Sendiri?
- SN010 – Amerika Ditatang,Islam Ditentang!
- SN011 – PILIHANRAYA : Sampai Bila Akan Menjadi Topeng Demokrasi
- SN012 – Hijrah Rasullullah Adalah Keluar Dari Darul Kufur Menuju Darul Islam
- SN013 – WIKILEAKS: Antara Bukti Kejahatan Pemimpin Dan Tajassus
- SN014 – Cabaran Dan Tentangan Sejurus Berdirinya Khilafah
- SN015 – Muhasabah Terhadap Harakah Islam Yang Mengakui Sistem Taghut
- SN016 – Tunisia Perlukan Khilafah, Bukan Sekadar Pertukaran Pemimpin
- SN017 – Mesir Bangkitlah Menuju Perubahan Hakiki Dengan Khilafah
- SN018 – Seruan Hizbut Tahrir Kepada Majlis Tertinggi Angkatan
- SN019 – Mempersiapkan Suasana Thalabun Nusrah Untuk Meraih Kekuasaan
- SN020 – Arab Saudi Dan Pengkhianatan Keluarga Saud
- SN021 – Kekejaman Diktator Libya & Keengganan Para Penguasa Kaum Muslimin Menolong Libya
- Sirah
- Tazkirah
- Tokoh2 Islam
- MMMP
- Sem 1 (Foundation)
- Case 1 (Chem of Life)
- Case 2 (Cell Structure)
- Case 3 (Active & Passive Movement)
- Case 4 (Transcription @ Translation)
- Case 5 (Vitamins,Fat & Water)
- Case 6 (Digestion & Absorption)
- Case 7 (Changes in Electrical Activity Caused by Damage)
- Case 8 (Lung Function,Environment & Epidemiology)
- Case 9 (Inherited Disease)
- Case Ten (Chemistry of Sugar)
- Pract/Osce
- Unseen Case (How's The Body is Regulated)
- Sem 2 (Life Cycle)
- Case 01 (Normal Pregnancy)
- Case 02 (Congenital Heart Disease)
- Case 03 (Thalassemia)
- Case 04 (Hypogonadism)
- Case 05 (Immunodeficiency-HIV/AIDS)
- Case 06 (Autoimmune-SLE)
- Case 07 (Autoimmune-Rheumatoid Arthritis)
- Case 08 (Breast Cancer)
- Case 09 (Osteoporosis)
- Case 10 (Menopause)
- Unseen Case (Ambiguous Genitalia)
- Xtra-Anatomy
- Sem 3 (Cardio-Respiratory)
- Sem 4 (Mind & Movement)
- Sem 5 (Body Metabolism)
- Sem 1 (Foundation)
- Posting (Elective)
- Society
- The Insider












