L2- Bronchial Asthma
Introduction:
•Immunity is not inherited.
•Humoral Immunity
- B lymphocytes – Antibody
•Cell mediated Immunity
- T lymphocytes – Macrophages
•Non-Specific immunity
- Neutrophils, Macrophages
•Primary response – slow, weak.
- Learning period, memory cells.
•Secondary response – rapid, strong
Immune Disorders:
- Immunodeficiency disorders (AIDS, antibody deficiency)
- Autoimmune disorders (SLE, Rheumatoid, Rheumatic fever)
- Hypersensitivity Disorders (allergy)
- excessive or altered reaction to an antigen producing adverse effects on the body. it is classified into 4 types
- Type-I (IgE)
- Type II-IgG
- Type III-Immune complex
- Type IV-Cell mediated.
Type I hypersensitivity reaction (Atopy)
Pathogenesis:-
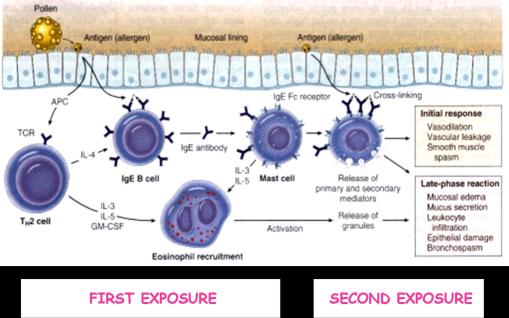
•First exposure to an antigen
-stimulation of B-lymphocytes to transform to IgE secreting plasma cells ( helped by CD4+ T-lymphocytes)
-IgE binds to the surface of mast cells and basophils
•Second exposure to the same antigen
-results in cross-linking of Ig E on the surface of mast cells
-Degranulation of the cells with release of chemical mediators
Chronic obstructive pulmonary disease (COPD)
•COPD is a disease state characterized by airflow limitation that is not fully reversible.
•The airflow limitation is usually both progressive and associated with an abnormal inflammatory response of the lungs to particles or gases.
•Classical COPDs
- Emphysema
- Chronic Bronchitis
- Bronchial Asthma
Bronchial asthma
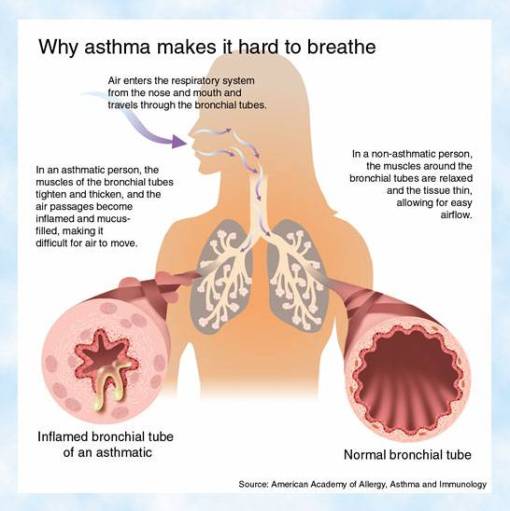
•Increased responsiveness of the bronchial tree to various stimuli that results in paroxysms of Bronchospasm
•reversible bronchospasm → later chronic bronchial inflammation, and obstructive lung disease
•It is episodic, reversible bronchospasm resulting from an exaggerated bronchoconstrictor response to various stimuli.
Incidence of asthma
•It is a common disease affecting 5% of adults and 7-10% of children.
•There has been a significant increase in the incidence of asthma in the Western world in the past three decades
Clinical
•it is manifested by recurrent episodes of wheezing, breathlessness, chest tightness, and cough.
•These symptoms are usually associated with bronchoconstriction and airflow limitation that is at least partly reversible, either spontaneously or with treatment.
•Between the attacks, patients may be virtually asymptomatic
•Rarely, a state of unremitting attacks, called status asthmaticus, proves fatal; usually, such patients have had a long history of asthma
-The attacks are triggered by exercise and cold or by exposure to an allergen to which the patient has previously been sensitized
Triggers of asthmatic episodes
- Allergens – pollen
- Pharmacological drugs such as aspirin,
- Environment pollution ozone, SO2, NO2
- Occupational- metal salts
- Infection- respiratory viruses
- Exercise
- Cold dry air
- Emotional stress
Pathogenetic Types:
- Extrinsic Asthma
- Intrinsic Asthma

•The concept that there are two types of asthma, extrinsic (due to allergy) and intrinsic ( due to constitutional factors) is not so sharp and there is much overlap between asthma with different triggers.
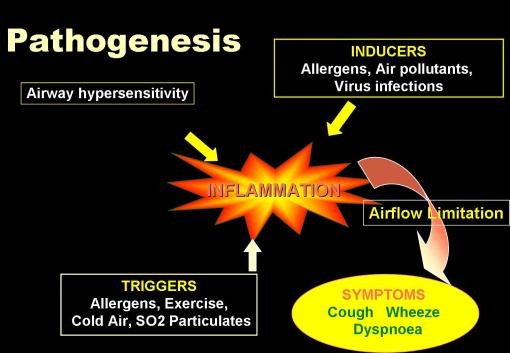
Pathophysiology

A- Pathogenesis of extrinsic (atopic) asthma
1- Meeting the specific allergen causes sensitization of CD4+ (T н2) cells resulting in release of cytokines (IL-4,5, and 13).
2- IL-4,5 and 13 cause
a. Stimulation of IgE production
b. Growth of mast cells.
c. Growth and activation of eosinophils.
3- Meeting the specific allergen for the second time results in an immune reaction which passes into two phases
- An early phase starting 30-60 min.after inhalation of the antigen then
- A late phase develops after 4-8 hours.
4- During the early phase, primary mediators are released. They include
- Leucotriens (C4,D4,and E4)
- Prostaglandins (D2,E2 and F2) .
- Histamine
- Platelet –Activating Factor
-These mediators produce
- bronchoconstriction
- vasodilatation
- increased vascular permeability
- increased mucin secretion.
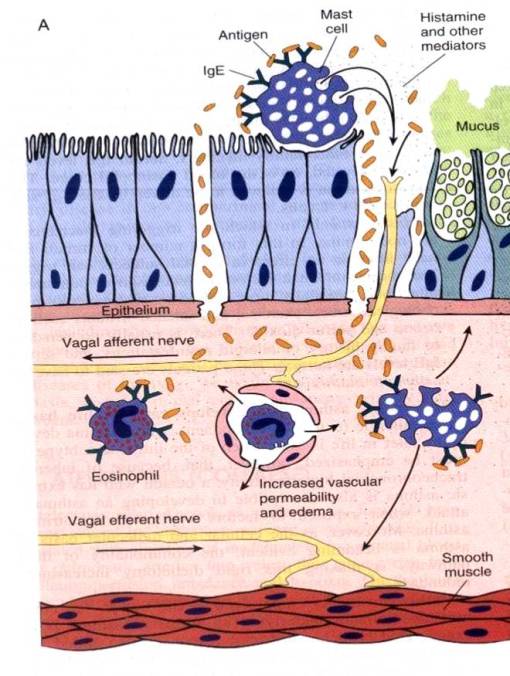 5- During the late phase secondary mediators are released including
5- During the late phase secondary mediators are released including
- Eosinophil and neutrophil chemotactic factors
- IL-4 &5
- Platelet Activating factor
- TNF
– These mediators produce eosinophil and neutrophil infiltration to the site of the lesion these cells produce;
a- More mediators that activate mast cells and intensify the initial response.
b. Epithelial cell damage.

B- Pathogenesis of intrinsic (nonatopic) asthma
Not fully understood, but a considerable overlap with extrinsic asthma is present and eosinophils seem to play an important role in both types. It may be:
- Virus-induced inflammation of respiratory mucosa lowers threshold of vagal receptors to irritants
- Aspirin-sensitive asthma
- Occupational asthma

 ATOPIC ASTHMA
ATOPIC ASTHMA
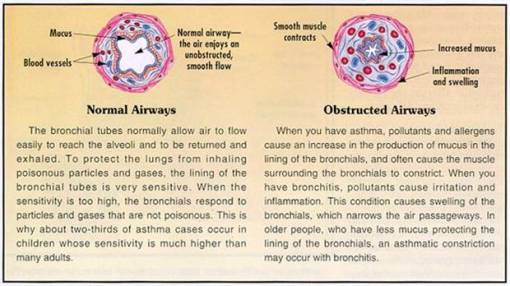
Lung Morphology in Asthma
- Mucous plugging
- Bronchospasm
- Obstruction
- Over inflation/Atelectasis
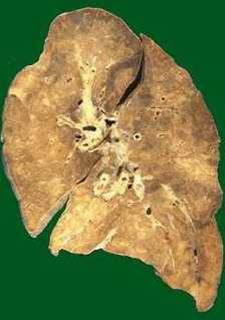
 Lung Hyperinflation in Asthma
Lung Hyperinflation in Asthma
 Thick bronchi with Mucous plugs
Thick bronchi with Mucous plugs

Microscopic Pathology
- Patchy necrosis of epithelium
- Sub-mucosal glandular hyperplasia
- Hypertrophy of bronchial smooth muscle
- Eosinophils, mast cells; lympho (TH2, CD4)
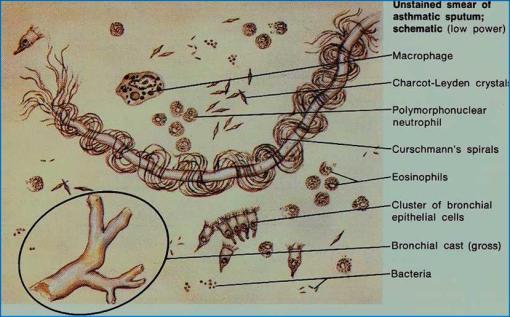
- Mucous plugs, Whorled mucous plugs (Curschmann’s spirals)
- Debris of eosinophils (Charcot-Leyden crystals)
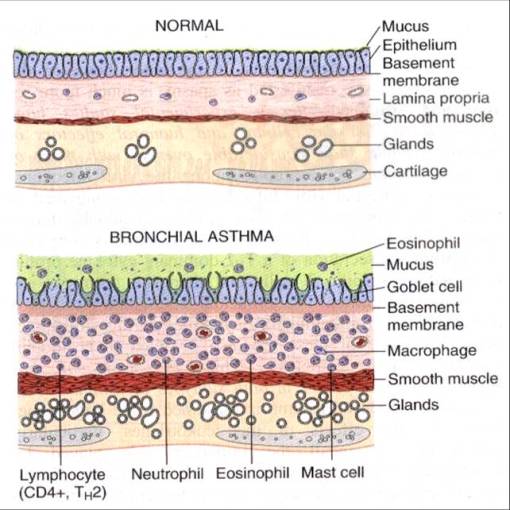

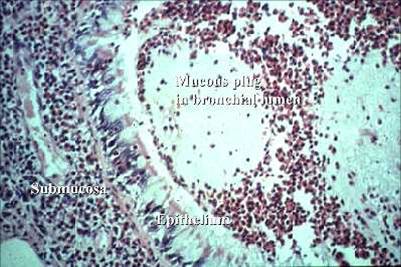
1) Obstructed Inflammed Bronchi
 2) Inflammation / Gland hyperplasia / Mucous plug in lumen (Bronchial Morphology)
2) Inflammation / Gland hyperplasia / Mucous plug in lumen (Bronchial Morphology)

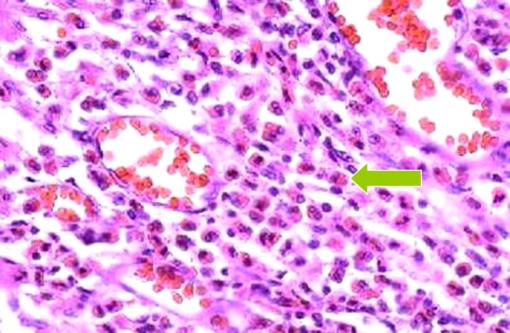
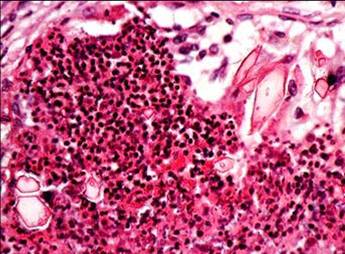
3) Inflammation / Mucous Plug / Eosinophils (Bronchial Morphology)
4) Eosinophils in Asthma:
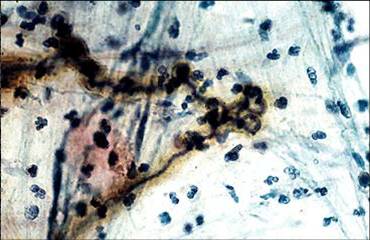
5) Curschmann’s spirals:

6) Mucous plugs with eosinophils and Charcot-Leyden crystals–bipyramidal hexagons fitted base to base
7) Mucous plugs with Curschmann’s spiral–fuzzy spiraled structures, derived from mucus
Complications
– At hemoglobin O2 saturations less than 85%, cerebral hypoxia, impaired brain functions , cyanosis and even death can occur.
Treatment
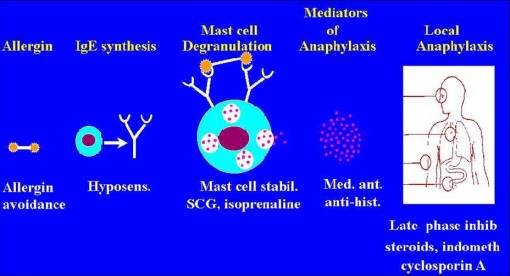
– Although asthma cannot be cured, appropriate management can control the disorder and enable people to enjoy a good quality of life.
– Some children with milder forms of asthma outgrow their symptoms with age
- Keep away from the triggers
- Medical and pharmacological treatment
- Two types of medication can be used
- Relievers or bronchodilators
Short-acting beta-agonists like salbutamol - Preventers Anti-inflammatory agents like corticosteroids
SUMMARY