L1- Physio Arterial Blood Pressure
Arterial blood pressure
Normal values
Factors affecting
How to measure
Regulation
The arterial Blood Pressure
It is the lateral force exerted by the moving column of blood on the lateral wall of arteries
Systolic blood pressure
-This is the maximum pressure created inside the arteries during ventricular systole due to rapid ejection of blood into the aorta.
-It normally ranges between 90 and 140 mmHg at rest.
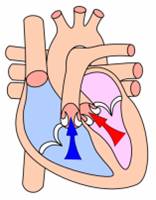
Diastolic blood pressure
It is the minimum pressure which remains inside the arteries at the end of ventricular diastole.
Diastolic blood pressure is normally between 60 and 90 mmHg at rest.
Pulse pressure
It is the difference between the systolic and diastolic blood pressures which equals about 40 mmHg.
The mean systemic ABP
This is the average pressure in the systemic arteries throughout the cardiac cycle.
It is calculated as:
Mean arterial blood pressure = diastolic pressure + 1/3 pulse pressure
Importance of ABP
1- It maintains sufficient pressure to keep the blood flowing.
2- It provides enough hydrostatic pressure inside the capillaries essential for the formation of interstitial fluid, urine, …. etc
Physiological Variations in ABP
1-Age
2-Sex
3-Race
4-Body built
5-Meals
6-Gravity
7-Emotions
8-Sleep
9-Exercise
10-Respiration
Measurement of ABP
-Direct measurement by cannulation of a large artery.
-Indirect measurement by Sphygmomanometer:
A-The palpation method
B-The auscultatory method

Factors that determine and maintain the ABP
1- The cardiac output
C O P = S V X H R
-Changes in the stroke volume with the HR constant affect the systolic more than the diastolic pressure.
-Changes in the HR with constant SV affect the diastolic more than the systolic blood pressure
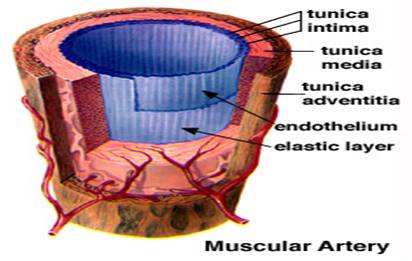
2-The peripheral resistance
Factors that determine the PR:
PR = VL/r4
A-The diameters of arterioles (r)
B-Viscosity of blood (V)
C-Length of the blood vessels (L)
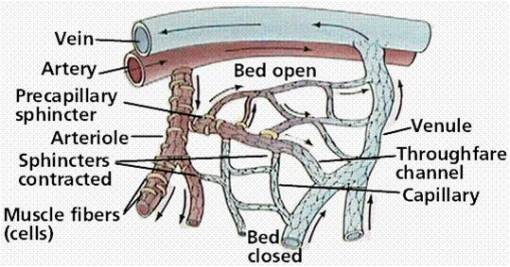
Regulation of diameter of arterioles
-The arterioles represent the main peripheral resistance in the vascular system.
-This appears from the marked decrease of ABP during the passage of blood in them (85 mmHg à 35 mmHg) compared to changes in ABP in different arts of the vascular system:
-arteries: 100 mmHg
-arterioles: 85 à 35 mm
-capillaries: 35 à 15
-venules : 10 mmHg
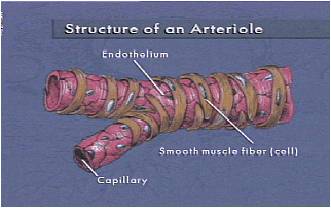
So, The diameter of arterioles is a very important factor in ABP regulation
The regulation of diameter of arterioles is achieved by:
1-Nervous regulation
2-Chemical regulation
3-Physical regulation
1-Nervous regulation
-This is achieved by continuous activity of VMC and the various factors affecting it.
-It is carried through the different vasoconstrictor and vasodilator nerves
2-Chemical regulation
1-Blood gases
a-Central on the VMC
b-Peripheral on arteriolar walls
2-Vasoactive substances:
a-Vasodilators e.g. metabolites, prostaglandins
b-Vasoconstrictors e.g. noradrenalin, ADH
3-Physical regulation
1-Application of cold (cold pressor test)
2-Aplication of heat
-vasodilatation
-Triple response
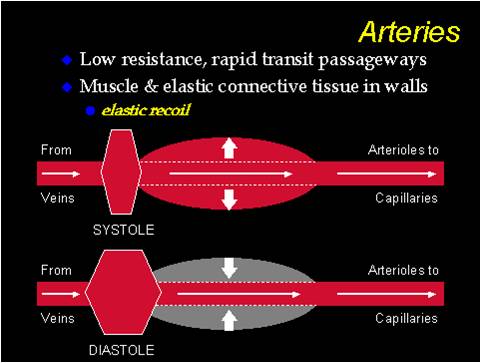
3-Elasticity of arteries
The elasticity of the aorta and its large branches buffer excessive changes in the arterial blood pressure during systole and diastole.
In atherosclerosis, there is marked increase in systolic and decrease in diastolic blood pressure resulting in a higher pulse pressure.
4-The total blood volume in relation to the capacity of the circulatory system
A- Changes in blood volume
B-Changes in the capacity of circulatory system
Regulation of Arterial Blood Pressure
A- Short-term (nervous) control mechanisms:
1- Arterial baroreceptors
These are spray type nerve endings that are present in the wall of carotid sinus, aortic arch, and to less extent in the wall of large arteries in the thorax and neck.
Baroreceptors are normally stimulated by the normal ABP forming the afferent limb of the Vagal tone.
Baroreceptors increase their discharge when the blood pressure increases. This leads to :
-Decrease in the heart rate.
-Arteriolar dilatation and venodilatation.
These reflexes restore the raised ABP back to its normal level.
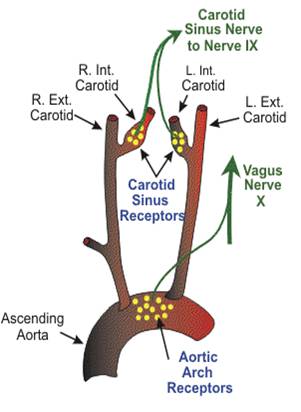
The arterial baroreceptors
2-The peripheral chemoreceptors
These are sensitive receptors to oxygen lack, carbon dioxide excess, or hydrogen ion excess.
They are located in the two carotid bodies and the aortic bodies.
Stimulation of chemoreceptors leads to:
-Arteriolar and venous constriction
-Acceleration of the heart
-Acceleration of respiration
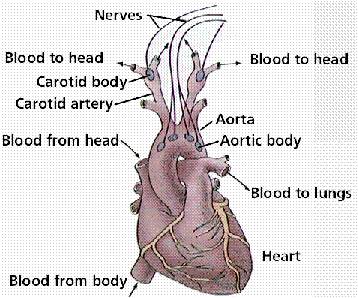
The peripheral chemoreceptors
3- Atrial baroreceptors
It is stretch receptors called also low pressure receptors or volume receptors.
Increased blood volume stimulates the atrial baroreceptors leading to:
A-reflex venodilatation
B- Vasodilatation of afferent renal arterioles
C-Impulses to the hypothalamus to decrease the secretion of ADH.
B- Intermediate-term control mechanisms
1-Capillary fluid shift mechanism
This mechanism corrects a change in blood volume by shifting of fluid between the plasma and the interstitial fluid.
A- An increase in blood volume
B-A decrease in blood volume
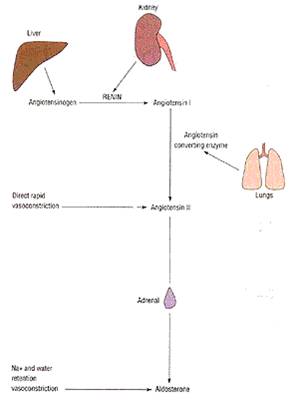
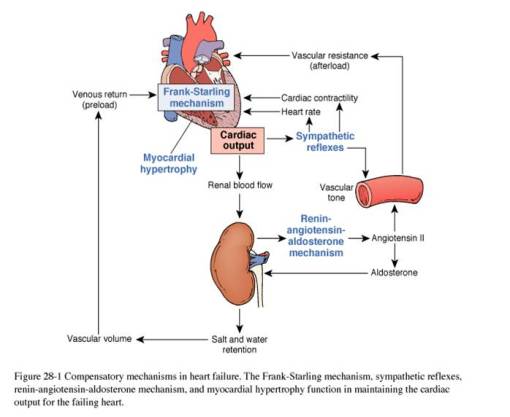
2-Renin-angiotensin mechanism
-A fall in arterial blood pressure decreases the renal blood flow. This releases renin which is a proteolytic enzyme.
-Renin changes angiotensinogen into Angiotensin I.
-Angiotensin I is changed in the lung by ACE into Angiotensin II.
-Angiotensin II is a strong vc substance and stimulates aldosterone secretion.
3- Atrial natriuretic peptide (ANP)
Stretch of atrial wall as a result of increased blood volume leads to release of atrial natriuretic peptide from the atria which:
-Act on the kidneys causing increased excretion of Na and H2O.
-Promotes vasodilatation
-Inhibit aldosterone, renin, and vasopressin
C- Long-term control mechanism
The renal – body fluid system
Increased ABP increases the rate at which the kidneys excrete both water and salt. This decreases the blood volume and therefore the arterial pressure.
Conversely, when the ABP falls too low, the kidneys retain fluids and the blood volume increases.
Hypertension
It is chronic elevation of the blood pressure above 140/90.
Types:
Primary Hypertension
Secondary Hypertension
Experimental Hypertension
This is the production of sustained high ABP in experimental animals.
It is used to investigate the hypotensive effect of various drugs and the possible causes that lead to a rise of ABP.
Experimental hypertension can be produced by the following methods:
1-Renal Ischemia
2-Denervation of the vasosensory areas
3-Afferent stimuli
4-Use of excess adrenocortical hormones
5-Use of excess vitamin D




great precise presentation