L2- Cardiac Output
Definition of the cardiac output (CO)
It is the quantity of blood pumped by each ventricle per minute. It is the quantity of blood pumped into the aorta each minute.
Cardiac output is perhaps the most important factor that we have to consider in relation to the circulation
Varies with age, sex, body activity
The Cardiac Cycle
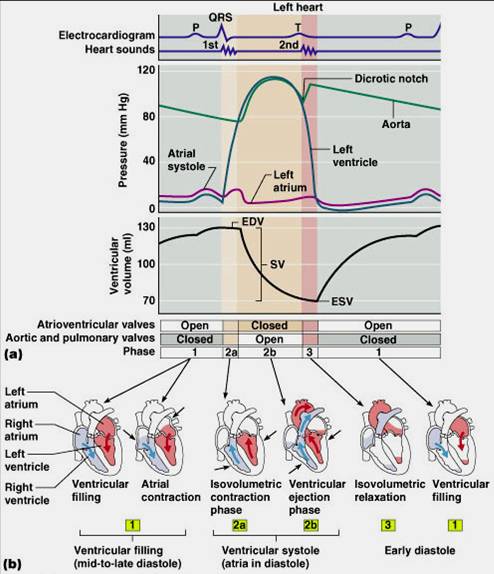
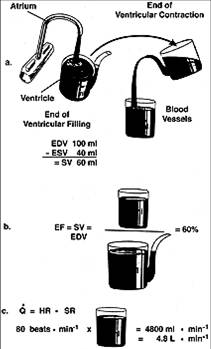
The end diastolic volume (EDV)
It is the volume of blood in the ventricle at the end of diastole.
It is about 110-130 ml
EDV is determined by Preload
The end systolic volume (ESV)
It is the volume of blood in the ventricle at the end of systole .
It is about 40-60 ml.
ESV is determined by after-load & contractility
The stroke volume (SV)
It is the volume pumped by each ventricle per beat.
It equals the difference between the end diastolic volume and the end systolic volume.
SV
= EDV-ESV
= 135-65 ml
=70ml
Factors increasing EDV will increase SV
Factors increasing ESV will decrease SV
Calculation of cardiac output
Cardiac Output in mL/min = heart rate (beats/min) X stroke volume (mL/beat)
An average person has a resting heart rate of 70 beats/minute and a resting stroke volume of 70 mL/beat.
The cardiac output for this person at rest is:
Cardiac Output = 70 (beats/min) X 70 (mL/beat)
= 4900 mL/minute.
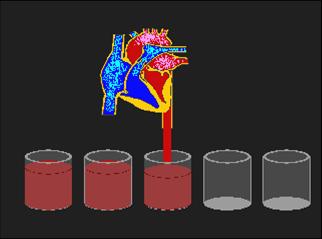
The total volume of blood in the circulatory system of an average person is about 5 liters . According to our calculations, the entire volume of blood within the circulatory system is pumped by the heart each minute (at rest). During vigorous exercise, the cardiac output can increase up to 7 fold (35 liters/minute)
Cardiac index
It is the cardiac output per square meter of body surface area.
For an adult it is about 3 L/min/m2.
It is used to compare the COP in different individuals
Ejection fraction (EF)
It is the percentage ratio of the SV to the EDV:
EF = SV/ EDV x 100
Normally it is about 65%. It is a sensitive index of myocardial contractility. It is decreased in heart failure.
It can be determined by echocardiography
Physiologic variations of the COP
1-Exercise
2-Metabolic state of the body
3-Body size
4-Age
5- Posture
6-Pregnancy
Measurement of cardiac output in man
(1) The direct fick’s principle
The amount of a substance taken up by an organ or by the whole body/min = arterial content – venous content X blood flow/min.
Requirements:
A- The O2 consumption/min
B- The O2 content in the venous blood
C- The O2 content in the arterial blood
Therefore, the COP
250/ (190-140)
= 250/ 50
= 5 liters /min
(2) Echocardiography:
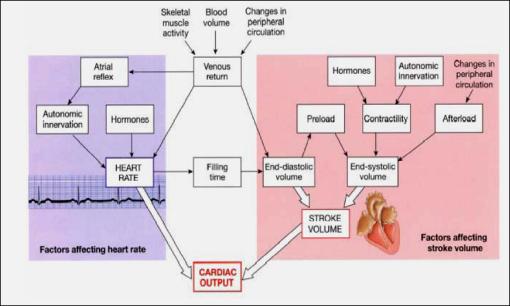
What are the Determinants of CO?
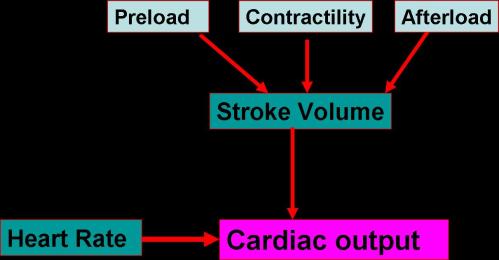
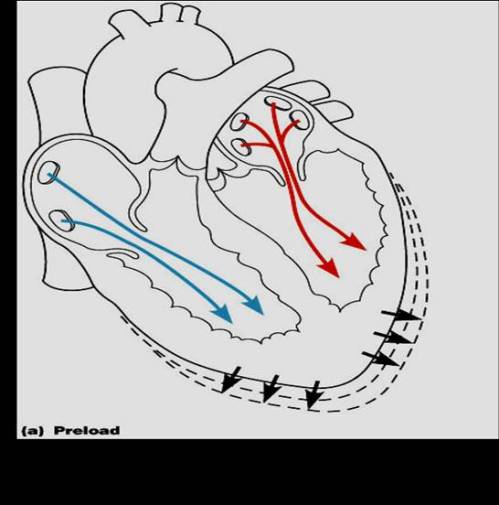
CO: Stroke V; Preload →EDV
•Preload is the initial stretch of ventricles prior to contraction
•Starling’s mechanism explains this on basis of Length-tension relationship which states that:
•The force of contraction increases with the increase in length (stretch) of cardiac muscles (within limits)
•This intrinsic ability of the heart to autoregulate CO (SV element) is called Heterometric Regulation; as the adjustment occurs following the change in muscle fibre length
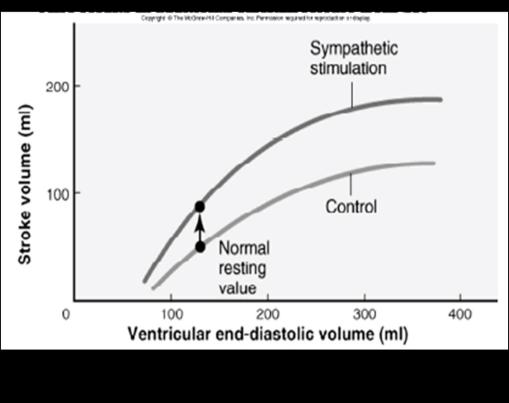
Frank-Starling Mechanism explaining effect of Preload on SV
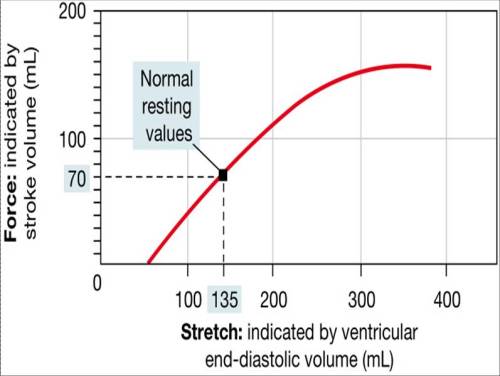
Heterometric Regulation
•A transient intrinsic regulatory mechanism
•According to Starling, an ↑ ↑in EDV will increase the length of cardiac muscle fibres→ ↑SV with slight increase in ESV
•Plays transient role in:
- Change of body posture from standing to recumbency (↑Bl flow from lower part of body)
- Sudden rise of ABP
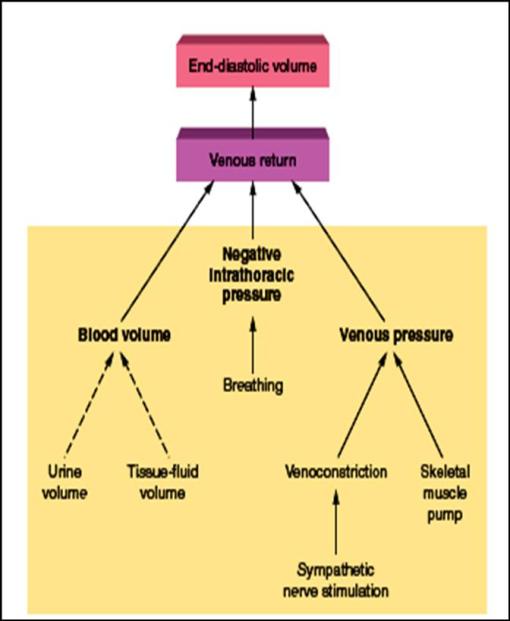
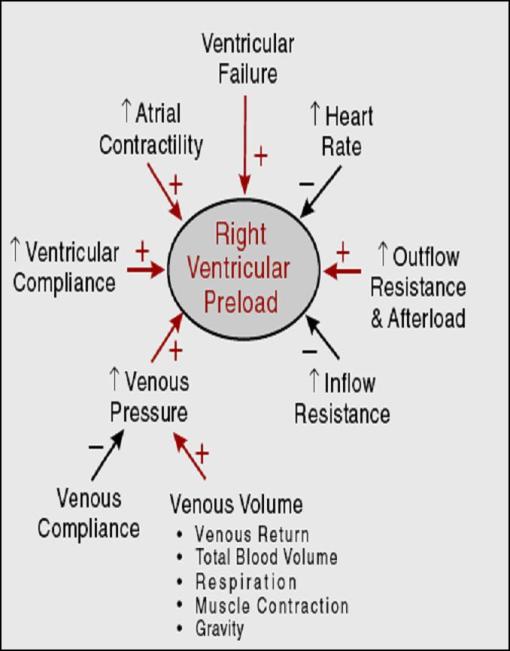
Preload (Ventricular filling) is determined by:
1.Venous Return (VR) coming to Rh Atrium
2.HR
3.Atrial Contractility
4.Ventricular compliance
5.Inflow resistance
6.Outflow resistance
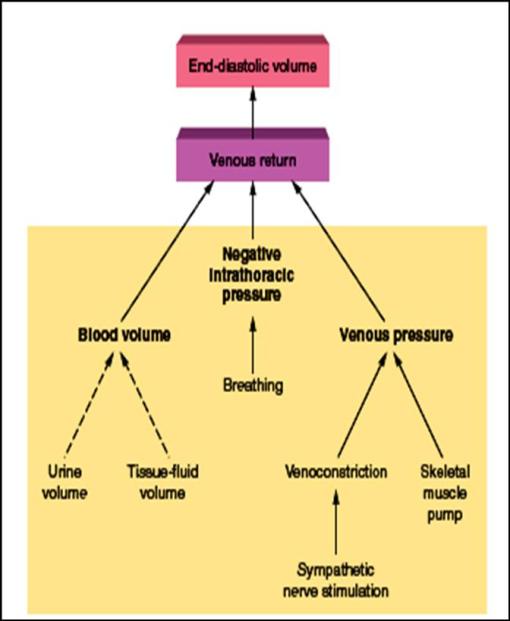
1- Venous Return
i.Venous pressure
ii.Skeletal muscle pump
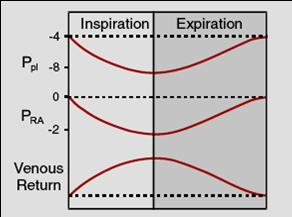
iii.Respiratory pump
iv.Gravity
v.Changes in peripheral circulation
1- Factors affecting Venous Return
i- Venous Pressure;
•Is the pressure gradient between mean circulatory filling pressure (MCP) in peripheral venules (~7 mm Hg; recumbent position) & the right atrial pressure (RAP: ~2 mm Hg; recumbent).
•It is the driving force for VR; so this gradient drives ~5L/min to right atrium
•Factors that ↑ MCP or ↓RAP will ↑VR
•Factors that ↓ MCP or ↑RAP will ↓VR
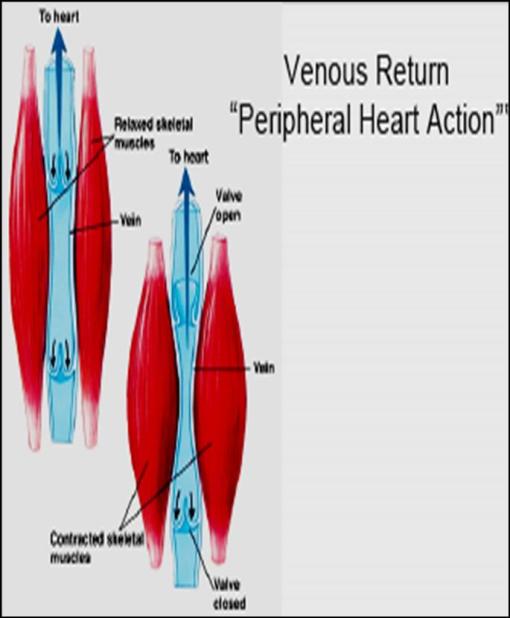
ii- Skeletal Muscle Pump
•The skeletal voluntary muscles act as peripheral hearts pumping blood against gravity
•During muscle relaxation, valves keep venous return to heart
•Muscle contraction message blood squeezing it towards heart.
iii- Respiratory Pump
•Inspiration ↑ negativity of intrathoracic pressure → ↑ suction of blood → ↑VR
•Expiration ↓negativity of intrathoracic pressure → ↓suction of blood → ↓VR
iv- Gravity
•In the recumbent position, gravity has no effect on VR
•In the standing position, gravity reduces VR from parts below the heart
•This effect is counteracted by:
- -Respiratory pump
- -Muscle pump
- -Valves in veins divide the large column of blood to small segments
v- Changes in peripheral circulation
•Arteriolar VD→ greater shunting of blood to venous side →↑VR
•Capillary dilatation →pooling of blood in capillaries →↓VR
(in severe burns, histamine release →shock due to major reduction in VR →extreme reduction in CO that may lead to death)
•Marked Venous dilatation → ↓VR (normally venous tone helps to prevent full distension & dilatation of veins).
2- Heart Rate (HR)
•Slow HR → ↑filling period → ↑EDV → ↑CO
• Marked increase in HR → shortening of diastole → ↓ EDV because ventricular filling occurs during diastole → ↓ CO
3- Inflow resistance
e.g. tricuspid stenosis ↓ atrial blood flow to Rh ventricle → ↓Preload → ↓ CO
4-Outflow resistance
e.g. pulmonary stenosis ↑ blood stagnation in Rh V → ↑preload
CO: Stroke Volume; Afterload
•Afterload is the load against which the heart must contract to eject blood, or it is the pressure that the ventricles must overcome to eject blood
•Is determined mainly by aortic pressure for Lt Ventricle & by pulmonary pressure for Rh Ventricle
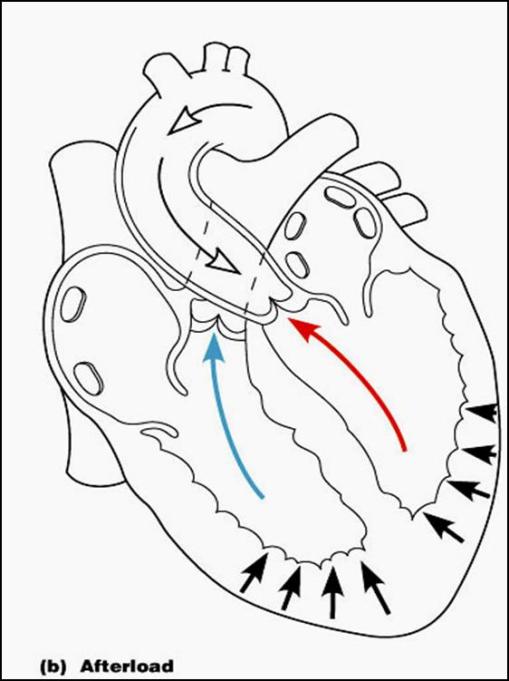
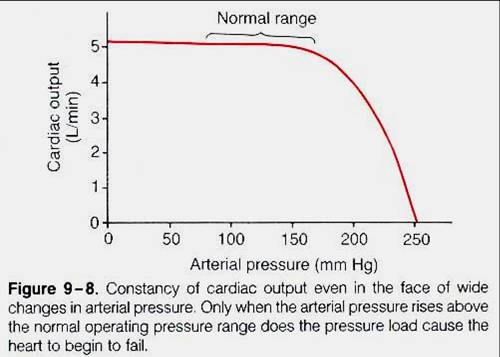
•Sudden increase in ABP (increased afterload) will impede ventricular ejection (shorter period of ejection)→ ↓SV → ↑ESV that is added to the next diastolic volume, thus ↑EDV; preload
•By Starling’s mechanism (Heterometric autoregulation), this will ↑force of contraction → ↑SV back to normal
Thus, the CO may not be changed but the Lt Ventricle is strained
CO: Stroke Volume; Contractility
•Contractility is the intrinsic ability of the ventricles to contract & pump blood
•Factors that enhance contractility → more pumping of blood; ↓ESV →↑SV
•Agents enhancing contractility are termed positive inotropic .e.g. Adrenaline, Noradrenalin, Digitalis, Glucagon, Corticosteroids, Xanthine derivatives
•Enhancing Contractility is induced by increased Ca influx into myocytes
•Acidosis, Increased extracellular K+ & Calcium channel blockers decrease contractility –
CO; Heart Rate
•Normal range of HR; 70-100 beats/min
•HR is an inherent property of cardiac muscle
•How much a change in HR affects CO depends on:
- -VR
- -The extent of change in HR
Change in HR with constant VR
•Moderate change in HR (either by increase or decrease) → no change in CO
•Because the change in HR will affect SV;
- An ↑in HR →↓filling time →↓EDV → ↓SV
- A decrease in HR→↑ filling time →↑EDV →↑SV
- Thus, CO remains constant
•Excessive change in HR will decrease CO
- If HR is >180 beats/m →great shortening of the diastolic filling time
•During muscle exercise, the increase in HR becomes the major player to increase CO & hence O2 supply to the tissues
•The increases VR will increase EDV
•↑ HR (BainBridge Reflex, Atrial reflex)
•Sympathetic stimulation during exercise enhances contractility →↑pumping of blood
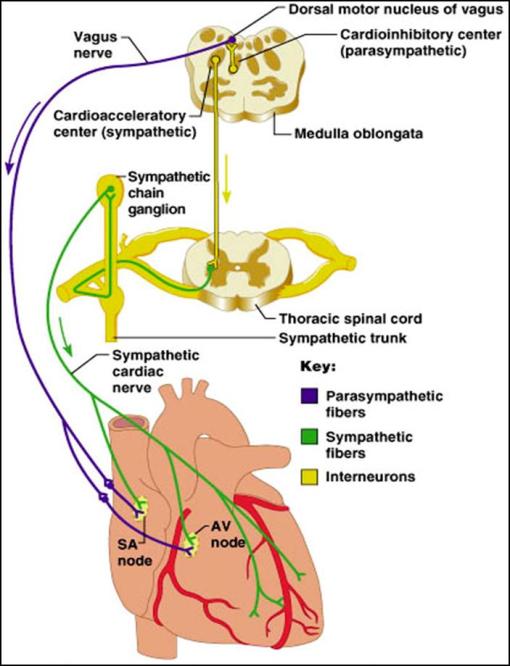
Factors affecting HR (Regulation of HR)
•Nervous & humoral regulation of HR
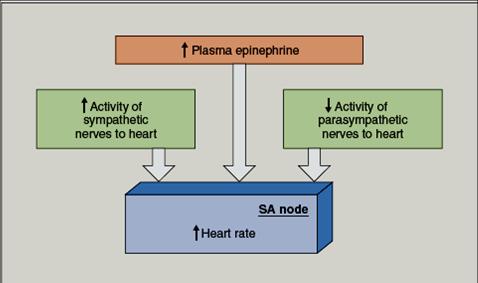
Autonomic NS; SNS & PNS
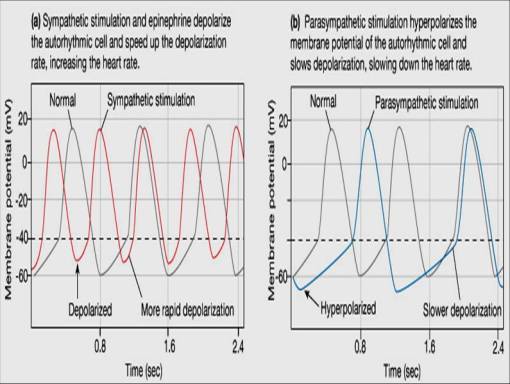
•SNS stimulation increases HR by enhancing Ca influx
•PNS stimulation decreases HR by enhancing K efflux
•Under resting conditions, HR is under control of PSN; Vagal tone
•Afferent impulses from higher centres modulate the autonomic regulation of HR;
-emotions, stress, exercise via cerebral cortex & posterior hypothalamus → sympathetic tachycardia
-Severe emotion & sleep via ant. Hypothalamus → PS bradycardia
Nervous Reflexes
•BainBridge Reflex;
Reflex increase in HR caused by an increase in VR
•McDowal’s Reflex;
decrease in VR as in haemorrhage→ an increase in HR as a part of sympathetic response
•Marey’s Law;
inverse relation between ABP & HR
Thus, an increase in ABP →↓HR thus, decreasing CO which lowers ABP
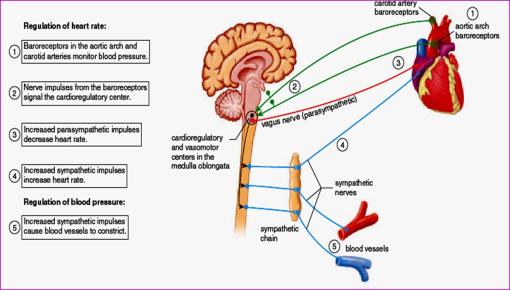
The Baroreceptor Pathway regulating relation between ABP & HR
How are the following can affect HR?
(Other factors regulating HR)
•Changes in blood gases
•Drugs & hormones
•Change in body Temperature
Factors affecting the COP
1- The venous return
2- The arterial blood pressure
3- The heart rate
4- The strength of ventricular contraction
I- Venous return (Preload)
It is the quantity of blood flowing from the veins into the right atrium each minute.
The venous return and the cardiac output must equal each other except for a few beats when blood is temporarily stored in or removed from the heart and lungs.
Factors influencing the venous return
1- The pumping action of the heart in forcing the blood into the blood vessels.
2- Skeletal muscle contraction (muscular pump)
3- Pressure gradient
4-Respiratory movements.
5-Gravity
6-Vascular system.
Effect of efficient venous valves
 NORMAL
NORMAL  DISEASED
DISEASED
II- Arterial Blood Pressure (Afterload)
Changes in arterial blood pressure have no effect on the cardiac output provided that the venous return remains constant
III- Heart rate
The effect of changes of heart rate on COP is influenced by:
– The amount of venous return
– The extent of changes in the heart rate
1-Changes of heart rate with constant VR
A- Physiological or moderate change of HR
COP
= HR X SV
= 50 X 100 = 5000 ml/min
= 100 X 50 = 5000 ml/min
B- Pathological or excessive changes in HR:
If the venous return is kept constant marked acceleration or slowing of the heart decreases the COP:
COP
= HR X SV
= 200X 20 = 4000 ml/min
= 30 X 130 = 3900 ml/min
2- Changes of HR with changes of VR (In muscular exercise)
When the VR is increased, the acceleration of the heart e.g. during muscular exercise will increase the COP due to:
-Increased EDV
-Decreased ESV
The cardiac output increases 7-8 folds.
IV- Strength of ventricular contraction
SV and COP are directly proportional to contractility
-When the ventricles contract more strongly, they pump more blood.
-On the other hand, if the myocardium is weakened, the COP decreases.
Regulation of cardiac output
The COP is regulated to meet the body requirements under different physiological condition to maintain adequate circulation.
There are two control systems:
1- Intrinsic system (autoregulation)
2- Extrinsic system
Intrinsic regulation
A-Heterometric autoregulation (Preload)
(Starling’law)
Physiologically this type is observed when a person goes from the standing position to the recumbent position
B-Homeometric autoregulation
If the augmented filling pressure to the heart persists, after few minutes of heterometric autoregulation, a different phenomenon is observed. It is characterized by:
1-Gradual return of the EDV to its normal level
2-The ESV is very much decreased than normal
3- The SV remains elevated
Extrinsic regulation
It regulates the COP by adjusting both the heart rate and stroke volume by:
A-Autonomic nervous system:
-Sympathetic Stimulation:
•Sympathetic NS (cardioacceleratory centre, CAC)
-stimulates heart
1- +ve chronotropic effect
2- +ve inotropic effect
-Parasympathetic Stimulation
•Parasympathetic innervation via vagus nerve (cardioinhibitory centre; CIC)
-inhibits cardiac properties (vagus does not supply ventricles)
The Cardiac Reserve
It is the difference between the cardiac work performed during rest and that performed at maximal exercise
•The difference between CO at rest & CO during exercise
•The heart uses its reserve whenever an extraload exists e.g. an increase in VR or ABP
•During exercise, CO can increase several folds due to the increase in EDV (Preload), contractility leading to an increase in SV +the increase in HR
•The heart increases its work through:
- -HR reserve (can ↑up to 180bpm without changing SV)
- -Stroke volume reserve; (preload & contractility)
↑ preload (EDV can ↑to 160 ml)
↑ contractility (↓ESV to 20ml)
So, CO
=160-20×180= ?L/min
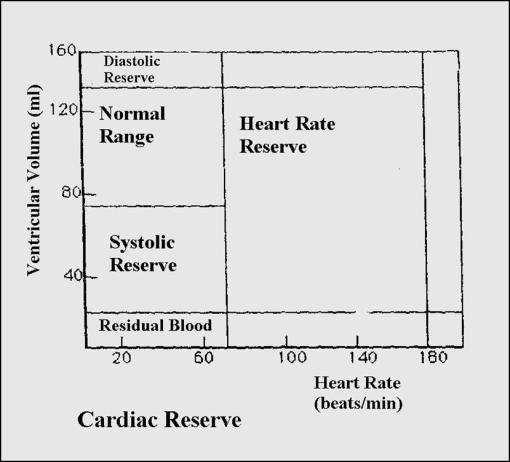
Mechanisms of cardiac reserve and Their limitations
1- Heart rate reserve
2-Stroke volume reserve
-Dilatation
-Sympathetic stimulation
3-Hypertropy
Summary CO



No trackbacks yet.