L1- Control of Alveolar Ventilation
Pulmonary Ventilation
•The exchange of air between atmosphere & alveoli
•Minute pulmonary ventilation = Tidal volume x RR= 500 ml x 12 cycles= 6L/min
•However, Effective Pulmonary ventilation or alveolar ventilation =350×12=4.2L/min
•Because 150 ml of air does not undergo gas exchange
Dead Space
•The space that contains the volume of air that does not undergo gas exchange
•Dead space is filled with inhaled air at the end of inspiration & with alveolar air at the end of expiration
•Types of Dead space:
– Anatomical; conducting zone of respiratory tract =150ml
– Alveolar ; non-functioning or partly functioning alveoli
– Physiological DS = anatomical D.S + alveolar D.S
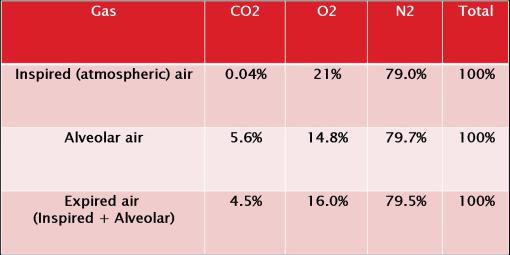
 •By studying this table, u can observe;
•By studying this table, u can observe;
•Why alveolar ventilation is the important
•Why the depth of ventilation (tidal volume) is more effective in increasing alveolar ventilation than an increase in RR
•The significance of dead space in some lung disease
FACTORS AFFECTING ALVEOLAR VENTILATION
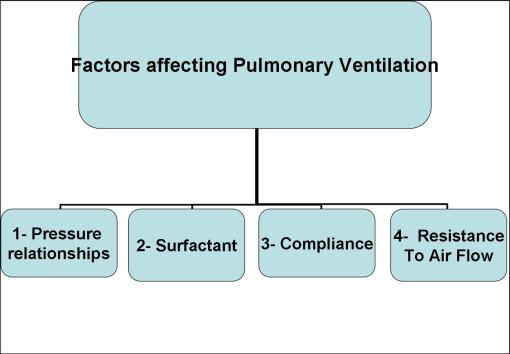
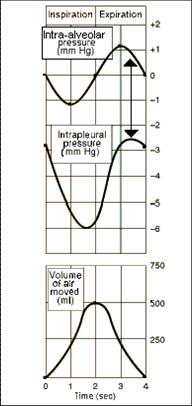
1- Pressure relationship in the thoracic cavity
2- Surfactant
-effect of surfactant in keeping the alveoli patent
3- Lung and chest compliance
Resistance to Air Flow
•It is responsible for approximately 80%-90% of total resistance forces during breathing.
•Contraction of respiratory muscles try to overcome forces that oppose lung expansion which are:
- elastic recoil of the lung
- frictional resistance; resistance to air flow imposed by tissues & airway
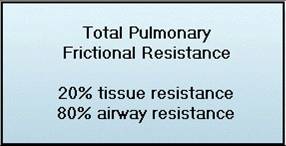
1) TISSUE RESISTANCE
•Constitutes ~ 20% of total resistance
•Friction form:
- movement of the lung over chest wall & pleura
- movement of lung lobes over each other
- movement of abdominal organs with the descent of the diaphragm
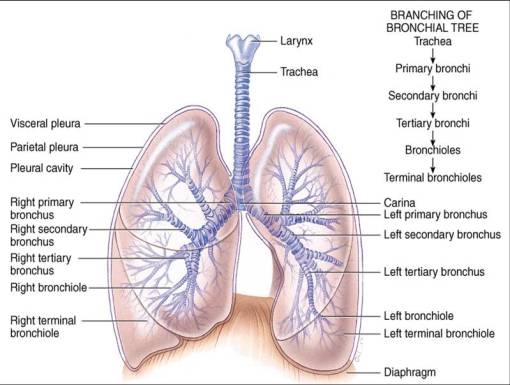
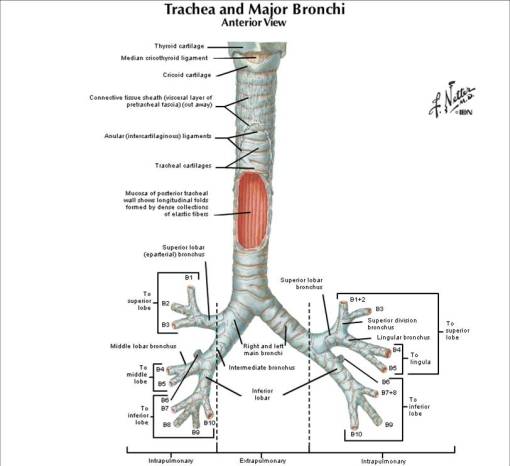
Cartilaginous airways: Trachea & Bronchi
•Cartilaginous horse-shaped rings give structural support for trachea & bronchi
•Has smooth ms layer supplied by parasympathetic nerve fibres (bronchoconstriction)
•Lined by mucous-secreting goblet cells & submucosal glands
Membranous airways: Bronchioles
•no fibrocartilaginous framework or submucosal glands
•Has a circular smooth muscle layer as bronchi
•Their support comes from elastic connective tissue fibres connecting them with surrounding lung tissue
2) Airway Resistance
•Responsible for ~80%
•Originates from:
- Friction between gas molecules each other & walls of air passages
•2 main factors controlling air flow through air passages are:
- Pressure gradient
- Resistance which is most affected by diameter of airways (R α 1/r4)
•Flow = Pressure gradient (P) / resistance (R)
•Very small P gradient is enough to move a large volume of air (1 mm Hg difference moves about 500 ml of air from atmosphere into alveoli)
•As the resistance is mostly affected by radius, so Airway diameter is the most important determining factor for airway resistance
FACTORS DETERMINING AIRWAY RESISTANCE
1- The rate of gas flow
•It is measured in liters per second.
•It equals the product of the velocity of the gas molecule in the airways and the cross sectional area of the airways.
2- The airway diameter
•It the most powerful determinant of resistance.
•The smaller the airway, the higher the resistance for any flow rate.
•CLINICAL SIGNIFICANCE
In COPD such as asthma, bronchitis and emphysema narrowing of the small airways occurs creating a very high airway resistance.
In order to maintain normal inspiratory and expiratory flow rates, COPD patients must generate much greater inspiratory and expiratory forces.
•CONTROL OF AIRWAY DIAMETER
I- NERVOUS
A- Sympathetic nerve stimulation to airways causes bronchodilation:
(i) Direct sympathetic nerve activation in humans causes only slight bronchodilation, because the adrenergic nerves do not actually innervate the bronchial smooth muscle.
(ii) The circulating adrenergic substances e.g. adrenaline, isoprenaline and adrenergic like drugs cause marked bronchodilation.
-This is because the bronchial smooth muscle contains a large number of B2 receptors .
-These receptors produce smooth muscle relaxation in response to these substances.
-Many B2 adrenergic drugs are now available via nebulizers for treatment of asthma .
B-Parasympathetic Vagus nerve stimulation to the lungs causes bronchoconstriction and increases the formation of mucus
-This narrows the airways and increases the resistance to air flow.
-Cholinergic activity is a major component in the pathogenesis of asthma in some individuals.
C- Nonadrenergic, Noncholinergic activity.
-The lungs is derived emberiologically in the foregut. Recently it has been recognized that many of the neuropeptides that control intestinal activity also control airway smooth muscle.
(i)Noncholinergic excitatory compounds e.g. substance P.
(i)Nonadrenergic inhibitory compounds e.g. prostaglandins and VIP
II- Chemical
A-Circulating hormones;adrenaline (B2 adrenoreceptors)
→bronchodilatation
B-Local mediators; histamine & slow reactive substance of anaphylaxis (SRS)
→ bronchoconstriction
C-Irritants; dust, smoke, air pollution, cold air →bronchoconstriction
III- Physical
A-Transpulmonary pressure
→ distending airway during inspiration (bronchodilatation) & bronchoconstriction during expiration
B-Local traction;
→ the elastic connective tissue connecting bronchioles to surrounding lung tissue make them dilate passively with inhaled air
•OTHER AIRWAYS RECEPTORS THAT MODULATE THEIR DIAMETER
1-Stretch receptors (Hering-Breuer reflex)
-They are Located in the small airways and are stimulated by inflation of the lungs.
-Their stimulation initiates the Herring-Breuer reflex that terminates the inspiration
2-Irritant receptors
-They are located in the large airways and are stimulated by smoke, dust or noxious gases.
-These receptors initiate reflexes that cause coughing, bronchoconstriction, mucus secretion and apnea (breath holding).
-Chronic exposure to irritants as in industrial atmospheres can lead to chronic bronchitis and other COPD with high airway resistance.
3-J receptors
-They are located in the pulmonary interstitium and are stimulated by distension of pulmonary capillaries.
-These receptors initiate reflexes causing rapid shallow breathing
4- Chest wall receptors
-They detect the force generated by the respiratory muscles during breathing. If the force increases excessively e.g. as a result of high airway resistance, it gives rise to the sensation of dyspnea.
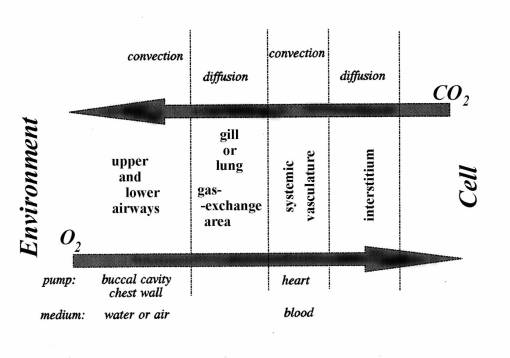
FACTORS AFFECTING GAS EXCHANGE
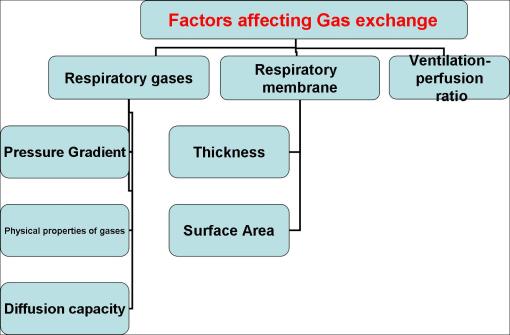
I- RESPIRATORY GASES
•Inspired air: This is atmospheric air
•The pressure of atmospheric air is 760 mmHg
•The atmospheric air on reaching the trachea , it becomes saturated with H2O vapour which has a pressure of 47 mmHg at normal body temperature.
•Now the total pressure of O2, CO2, N2 in the respiratory tract is only 713 mmHg.
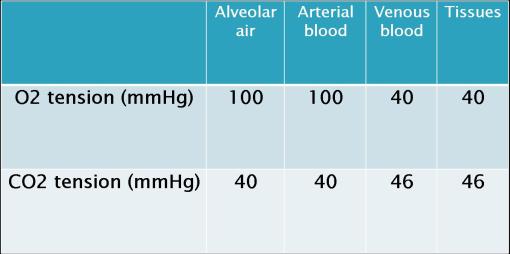
•The partial pressure of a gas in a mixture of gases = % of gas in mixture x total pressure of the mixture:
-O2 in atmospheric air has a pressure of 21/100 x 760 = 159 mmHg
-At high altitude the atmospheric pressure decreases e.g. to 400 mmHg . So, the oxygen pressure becomes 21/100 x 400 = 84 mmHg
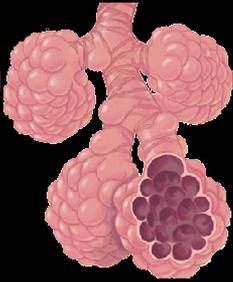
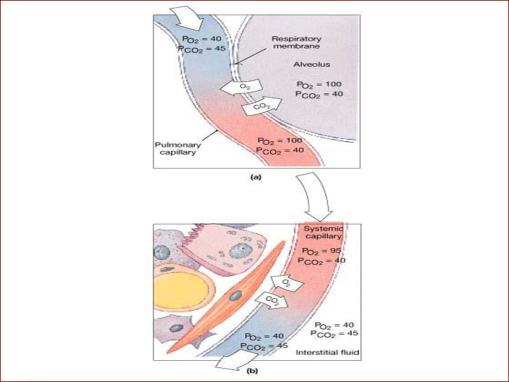
•Alveolar air:
This is the air present in the alveoli, air sacs, alveolar ducts and respiratory bronchioles. This air undergoes gas exchange with blood in pulmonary capillaries.
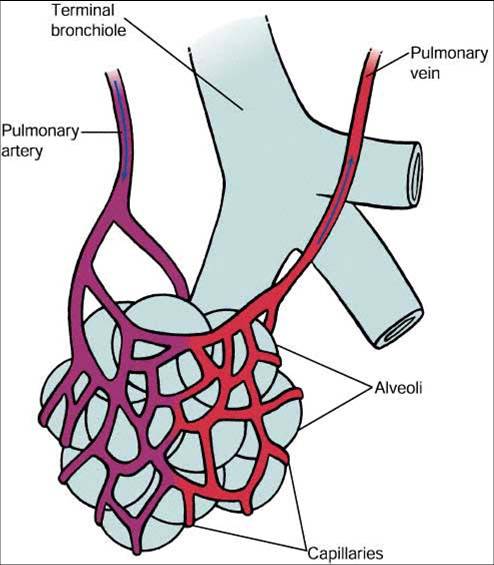 alveolar air exchange w/ pulmonary capillaries
alveolar air exchange w/ pulmonary capillaries
 alveolar gas exchange through the respiratory membrane
alveolar gas exchange through the respiratory membrane
•Expired air:
Mixture of alveolar air and the air in the respiratory passages. It contains more O2 but less CO2 than alveolar air.
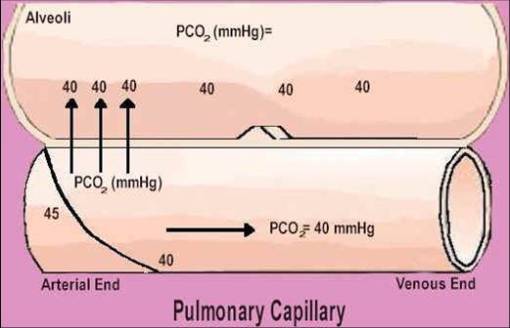
•Pressure Gradient
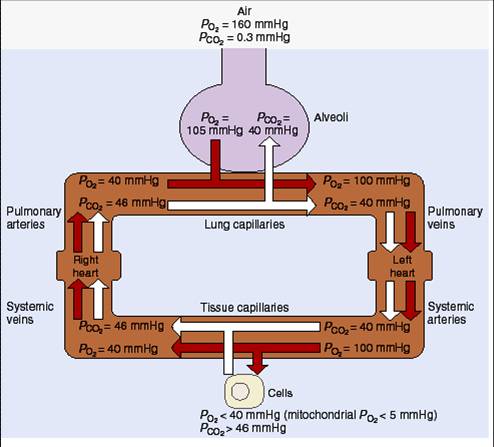
•Different respiratory gases composition
•Alveolar gases exchange
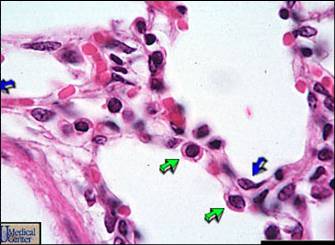
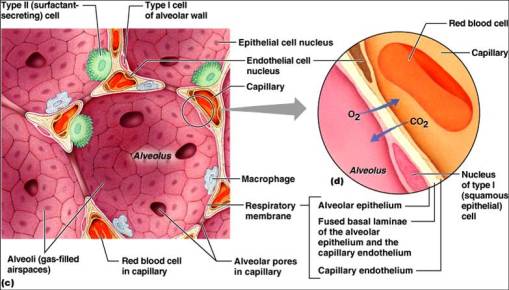
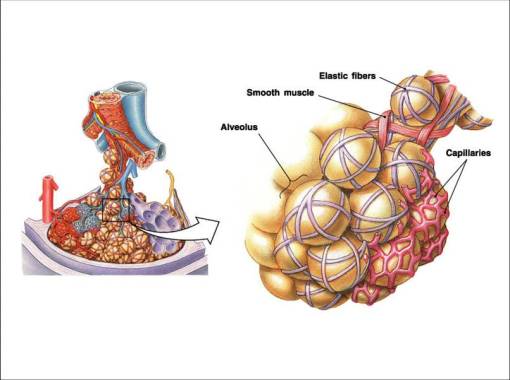
II- Respiratory Membrane
1- Thickness (normal: 0.2-0.6um)
•↑ thickness → ↓ gas diffusion (pulmonary oedema)
2- Surface area (normal: 60 m2)
•↑surface area →↑ rate of gas exchange
•↓ surface area→↓ rate of gas diffusion (emphysema, lobectomy)
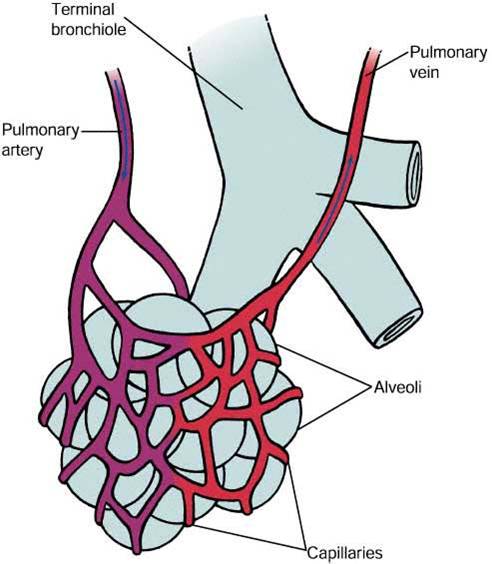
III(1)- VENTILATION PERFUSION RATIO
•This is the ratio between effective alveolar ventilation and pulmonary blood flow per minute.
•The normal alveolar ventilation in an adult is 4L/min (350 x12). The total perfusion of lung is 5L/min. So, the ratio is about 0.8. This differs from one part of the lung to another.
Physical properties of Gases
•When a gas is moving from gas mixture to be dissolved in a liquid, the amount will depend on its partial pressure & its solubility
•O2 & CO2 are lipid soluble, so they diffuse easily through cell membrane
•However, the CO2 solubility is greater than O2 .Thus, the Diffusion rate of CO2 is higher than that of O2 by 20 times although the pressure gradient for CO2 is less
•The Diffusion Capacity:
- For O2 = 20ml/min/mm Hg
- For CO2 = 400ml/min/mm Hg
•Alveolar gas exchange
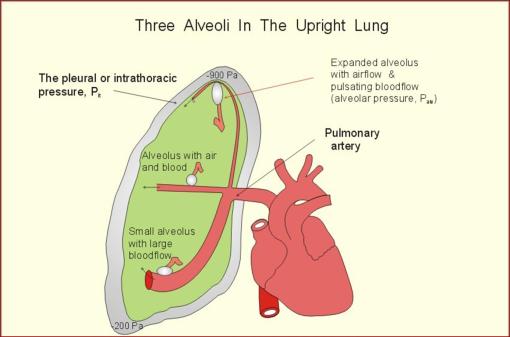
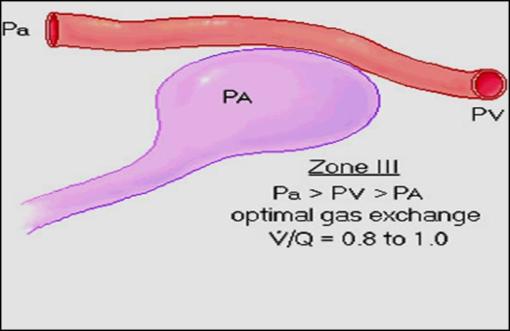
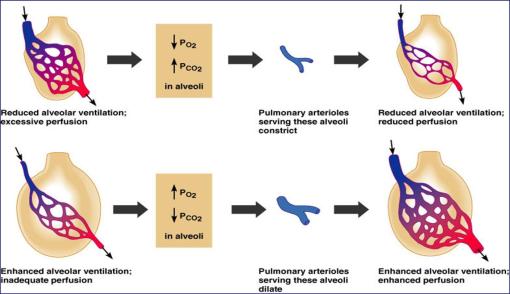
III(2)- VENTILATION PREFUSION BALANCE
•The lung is divided into 3 zones of ventilation perfusion balance by considering the relation between:
– Alveolar pressure (PA)
– Pulmonary artery pressure (Pa)
– Pulmonary venous pressure (Pv)
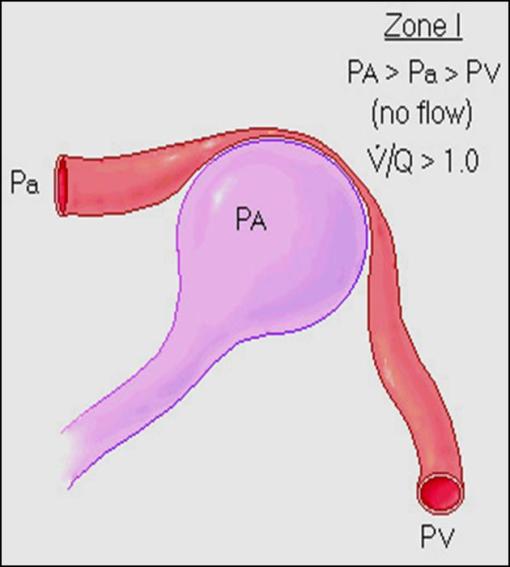
ZONE (I)
•At the top of the lung (APEX) where:
PA > Pa > Pv
•This zone is hyperventilated hypoperfused
V/p = 3.3
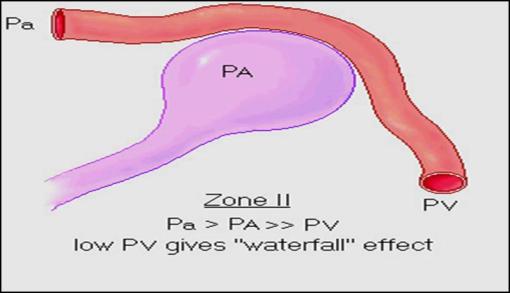
ZONE (II)
•In the middle of the lung where:
The pulmonary artery pressure Pa exceed the PA :
(intermittent flow)
Pa > PA
ZONE (III)
•Venous pressure now exceeds alveolar pressure and blood flow increases down this region:
PV> PA
•This region is hyperperfused
V/p ratio = 0.6
Local regulatory mechanisms to correct for mismatch



No trackbacks yet.